Expert Insights on Preventing Gestational Diabetes During Pregnancy
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
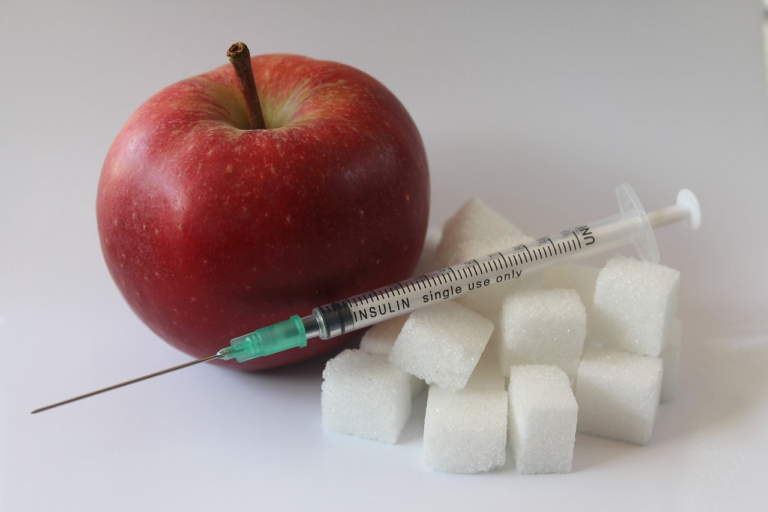
1. Introduction to Gestational Diabetes
Gestational diabetes mellitus (GDM) represents a significant and growing concern in maternal health, characterized by high blood sugar levels that develop during pregnancy and typically resolve after childbirth. A comprehensive understanding of gestational diabetes is crucial, as it affects a notable percentage of pregnant women worldwide, leading to potential complications for both the mother and the developing fetus. This introduction aims to provide an extensive overview of gestational diabetes, emphasizing its prevalence and the importance of preventive measures for safeguarding maternal and fetal health.
Gestational diabetes occurs when a woman’s body is unable to produce enough insulin to meet the increased demands during pregnancy, leading to hyperglycemia, or elevated blood glucose levels. This condition not only presents risks during pregnancy but can also have long-term health implications for both mother and child. Therefore, awareness and early intervention are key in managing and mitigating these risks.
Prevalence of Gestational Diabetes Among Pregnant Women
In recent decades, the prevalence of gestational diabetes has been on the rise. This trend can be attributed to various factors, including increased maternal age, obesity rates, and other underlying health conditions that affect glucose metabolism. Studies indicate that gestational diabetes affects approximately 7-10% of pregnancies globally, with variations based on population demographics and screening methods. The condition is typically diagnosed between the 24th and 28th weeks of pregnancy through specific glucose tolerance tests.
The rising prevalence poses a substantial challenge for healthcare systems worldwide, necessitating more rigorous screening protocols and healthcare policies to manage and mitigate the impact of gestational diabetes. Addressing this issue is essential not only from a public health perspective but also for improving pregnancy outcomes and reducing long-term healthcare costs.
Importance of Preventing Gestational Diabetes for Maternal and Fetal Health
Preventing gestational diabetes is imperative for ensuring the health and well-being of both the mother and the fetus during and after pregnancy. Unsupported gestational diabetes can lead to various complications, such as preeclampsia, cesarean delivery, and the development of type 2 diabetes later in life for the mother.
For the fetus, unmanaged gestational diabetes can result in excessive birth weight (macrosomia), preterm birth, and increased risk of developing metabolic conditions in childhood. Proactively preventing gestational diabetes through lifestyle modifications, regular monitoring, and, if necessary, medical intervention, can significantly minimize these risks.
- Preeclampsia: A condition characterized by high blood pressure and signs of damage to another organ system, often the kidneys, which affects both maternal and fetal health if not properly monitored.
- Macrosomia: Infants born with excessive birth weight are more likely if gestational diabetes is present, increasing the likelihood of birth injuries and complications during delivery.
- Neonatal Hypoglycemia: Babies born to mothers with gestational diabetes may experience low blood sugar levels after birth, requiring careful monitoring and management.
By understanding the significance of gestational diabetes and its implications, healthcare providers can better advise and support women in reducing their risk, ensuring healthier outcomes for themselves and their children.
Introduction to Expert Perspectives and Insights
To shed more light on gestational diabetes, experts in the field provide crucial insights into effective management and preventive strategies. Through a variety of perspectives that include nutritional advice, lifestyle adjustments, and medical interventions, these professionals contribute to a broader understanding of how to combat this condition effectively.
- Dr. Jane Smith, an obstetrician, highlights the impact of individualized care plans for mothers diagnosed with gestational diabetes, emphasizing the importance of maintaining regular prenatal check-ups.
- Nutritionist John Doe discusses dietary modifications essential for maintaining optimal blood glucose levels during pregnancy, recommending balanced meals and regular physical activity.
- Endocrinologist Dr. Mary Johnson explores the role of insulin therapy and other medications for those unable to control blood sugar levels through diet and exercise alone.
Integrating these expert insights into a comprehensive care plan empowers expecting mothers to navigate gestational diabetes proactively, safeguarding their health and the health of their unborn children.
In conclusion, while gestational diabetes presents unique challenges during pregnancy, an informed approach focusing on prevention and management can lead to favorable outcomes. With the rise in its prevalence, it is imperative to continue research and education efforts, supporting healthcare providers and mothers-to-be in their journey toward healthy pregnancies and beyond.

2. Understanding the Risk Factors
Understanding the risk factors associated with gestational diabetes is crucial for expecting mothers. Gestational diabetes, a condition characterized by high blood sugar levels during pregnancy, can lead to complications if not managed effectively. Luckily, with expert insights and timely interventions, these risks can often be mitigated. In this segment, we’ll delve into the common risk factors for gestational diabetes, provide expert guidance on identifying and managing these risks early in pregnancy, and discuss strategies for minimizing risk through lifestyle and dietary modifications.
Common Risk Factors for Gestational Diabetes
- Obesity: Excessive body weight is a significant risk factor for gestational diabetes. Women with a body mass index (BMI) of 30 or higher are more likely to experience this condition.
- Family History: A family history of diabetes can predispose you to gestational diabetes. Understanding your genetic background helps anticipate potential risks.
- Previous Gestational Diabetes: If you have had gestational diabetes in a previous pregnancy, the likelihood of developing it in subsequent pregnancies increases.
- Sedentary Lifestyle: Lack of physical activity can contribute to insulin resistance, increasing the risk of gestational diabetes.
- Age: Pregnant women over the age of 25, especially those over 35, are at a higher risk of developing gestational diabetes.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS are at an elevated risk due to hormonal imbalances that affect glucose regulation.
- Ethnicity: Certain ethnic groups, including Hispanic, African American, Native American, and Asian, face higher risks for gestational diabetes.
Expert Insights on Identifying and Managing Risks Early in Pregnancy
Early identification of risk factors can significantly improve management strategies for gestational diabetes. Consulting with healthcare professionals as soon as you suspect a risk is beneficial. Here are some expert insights into managing gestational diabetes risks:
-
Regular Screening:
- Screening involves initial glucose tests to measure blood sugar levels. If you are in a high-risk category, your doctor may recommend screening as early as your first prenatal visit.
-
Monitoring Blood Sugar Levels:
- Regular monitoring helps keep track of glucose levels, thereby managing and adjusting dietary and activity habits accordingly.
-
Individualized Care Plans:
- Working with healthcare professionals to develop a personalized care plan is essential. This includes scheduled check-ups, blood tests, and consultation sessions.
-
Risk Factor Assessment:
- An assessment of personal and family medical history, BMI, and other health aspects forms the basis for managing gestational diabetes.
Strategies for Minimizing Risk Through Lifestyle and Dietary Changes
Proactive lifestyle changes and dietary modifications can significantly reduce the risk of developing gestational diabetes. Here are strategic measures to consider:
-
Adopt a Balanced Diet:
- Focus on whole foods, fruits, vegetables, lean proteins, and whole grains. These foods help maintain steady blood sugar levels.
- Avoid highly processed foods, sugary snacks, and drinks that spike blood sugar levels.
-
Exercise Regularly:
- Engage in at least 30 minutes of moderate exercise, such as walking or swimming, most days of the week to enhance insulin sensitivity.
- Consult your healthcare provider to tailor exercises appropriate for your pregnancy stage.
-
Maintain a Healthy Weight:
- Aim to achieve and maintain a healthy weight before and during pregnancy as part of minimizing gestational diabetes risk.
-
Stress Management:
- Employ stress-relief techniques such as yoga, meditation, and deep-breathing exercises. Elevated stress levels can indirectly influence blood sugar levels.
-
Adequate Sleep:
- Ensure you get sufficient sleep, typically 7-9 hours per night, to support healthy metabolic processes and hormone regulation.
In summary, understanding and managing the risk factors for gestational diabetes is crucial for a healthy pregnancy journey. By identifying these risks early on and implementing strategic lifestyle and dietary changes, the potential impact of gestational diabetes can be mitigated. Consultation with healthcare professionals, personalized care plans, and dedication to a balanced lifestyle are fundamental to reducing risk and ensuring the wellbeing of both mother and child.

3. Nutritional Guidelines and Dietary Management
Gestational diabetes is a prevalent pregnancy complication, affecting a significant number of expecting mothers worldwide. This condition necessitates careful attention to dietary management and proper nutritional guidelines to ensure the health and well-being of both the mother and the unborn child. In this article, we provide expert-recommended nutritional guidelines to prevent gestational diabetes, highlight the importance of a balanced diet, and offer nutrient recommendations. Additionally, we share valuable meal planning tips and advice from experienced nutritionists.
Expert-Recommended Nutritional Guidelines to Prevent Gestational Diabetes
Nutritional guidelines play a crucial role in preventing gestational diabetes. These guidelines entail making informed dietary choices that can help manage blood sugar levels effectively. Here are some expert recommendations:
- Prioritize complex carbohydrates: Incorporating complex carbohydrates such as whole grains, legumes, and vegetables can help maintain stable blood sugar levels. They release glucose slowly into the bloodstream.
- Include lean proteins: Consuming adequate amounts of lean proteins such as chicken, fish, tofu, and legumes can promote satiety and maintain muscle health.
- Choose healthy fats: Opt for healthy fats like avocados, nuts, seeds, and olive oil. These fats can support cellular health without spiking blood sugar levels.
The Importance of a Balanced Diet and Specific Nutrient Recommendations
A balanced diet is imperative for overall health and particularly crucial during pregnancy. A well-balanced diet provides essential nutrients that support fetal development and maternal health. Here are some key nutrients to focus on:
- Fiber: Increasing fiber intake helps regulate blood sugar levels and improve digestion. Foods high in fiber include fruits, vegetables, and whole grains.
- Calcium: Calcium is vital for fetal bone development. Good sources include dairy products, leafy greens, and fortified non-dairy alternatives.
- Iron: Iron supports increased blood volume during pregnancy. Incorporate foods like lean meats, beans, and fortified cereals to meet iron needs.
- Folic Acid: Essential for reducing neural tube defects, folic acid can be found in leafy greens, citrus fruits, and fortified grains.
- Omega-3 Fatty Acids: Supportive of fetal brain and eye development, omega-3s can be sourced from fish, flaxseeds, and walnuts.
Meal Planning Tips and Advice from Nutritionists
Effective meal planning is a cornerstone of managing gestational diabetes. By planning meals ahead, mothers can ensure balanced nutrition and consistent glucose levels. Here are some practical tips from nutritionists:
- Portion control: Keep an eye on serving sizes to avoid overeating, especially foods high in carbohydrates.
- Frequent small meals: Eating small, frequent meals throughout the day can prevent large fluctuations in blood sugar levels.
- Hydration: Staying well-hydrated aids in digestion and metabolic processes. Aim for at least 8-10 glasses of water daily.
- Prepare balanced snacks: Healthy snacks like nuts, yogurt, or a piece of fruit can keep blood sugar levels stable between meals.
- Limit sugar and refined carbs: Minimize intake of sugary foods and refined carbohydrates that can cause spikes in blood glucose.
By adhering to these nutritional guidelines and meal planning suggestions, expecting mothers can significantly reduce their risk of gestational diabetes and support their health and their baby’s development. Always consult with a healthcare provider or a registered dietitian for personalized dietary advice tailored to individual needs and health conditions.
4. Exercise and Physical Activity Recommendations
Staying active during pregnancy is crucial for both the mother and the developing baby. Understanding the role of physical activity in reducing the risk of gestational diabetes can empower expectant mothers to embrace a healthier lifestyle. In this segment, we will explore how exercise benefits pregnancy, offer expert-approved exercises and activity levels, and provide tips on integrating physical activity safely during pregnancy.
Role of Physical Activity in Reducing the Risk of Gestational Diabetes
Gestational diabetes mellitus (GDM) is a common complication that occurs during pregnancy, characterized by carbohydrate intolerance resulting in hyperglycemia. Regular physical activity plays a significant role in managing weight gain, improving insulin sensitivity, and enhancing overall health, which collectively contribute to minimizing the risk of developing GDM.
- Improved Insulin Sensitivity: Exercise helps muscles use glucose more effectively, reducing insulin resistance that commonly occurs in gestational diabetes.
- Weight Management: Keeping weight gain within recommended limits can lower the risk of developing GDM and other related pregnancy complications.
- Enhanced Circulation: Physical activity promotes better blood circulation, which can prevent potential issues related to blood sugar fluctuations.
Expert-Approved Exercises and Activity Levels for Pregnant Women
Engaging in physical activities that are appropriate for pregnancy can offer numerous benefits without posing risks to the mother or fetus. It’s important to choose exercises that cater to each individual’s fitness level and pregnancy stage.
Recommended Exercises
- Walking: A simple yet effective low-impact exercise that helps boost cardiovascular health without undue stress on the joints. Pregnant women can aim for at least 30 minutes of walking on most days.
- Swimming: This full-body workout is gentle on the body while increasing muscle tone and strength. It also provides relief from pregnancy-related aches and promotes relaxation due to the buoyant nature of water.
- Pregnancy Yoga: Focusing on breathing, flexibility, and mental wellness, yoga can help relieve stress, improve posture, and strengthen essential muscle groups.
- Stationary Cycling: Provides a safe way to engage in cardiovascular exercise with minimal impact on the pelvis and back.
- Resistance Training: Light weights or resistance bands can help maintain muscle tone, support joint health and prepare the body for labor.
It is vital to receive clearance from a healthcare provider before starting any new exercise routine during pregnancy and to tailor activities based on individual conditions and doctor recommendations.
Activity Levels
Physical activity levels should be customized based on pre-pregnancy fitness levels and any existing health conditions. Here are general guidelines for safe exercising during pregnancy:
- Beginners: Start with 15 minutes of high-quality, low-impact activities three times a week, and gradually progress to 30 minutes as comfort and stamina improve.
- Regular Exercisers: Continue with regular activity, adjusting the intensity to match energy levels and avoiding high-impact or high-risk activities.
- Athletic Individuals: Modify high-intensity routines to prioritize safety, avoiding exercises that may challenge the body’s stability or strain the abdominal area.
Tips on Integrating Physical Activity Safely During Pregnancy
Exercising safely is essential to ensure the well-being of both mother and baby during pregnancy. Here are some essential tips to help integrate physical activity effectively.
- Listen to Your Body: Pay attention to physical responses and modify activities to avoid overexertion. Signs to watch for include dizziness, shortness of breath, and joint or muscle pain.
- Stay Hydrated: Proper hydration is crucial to support increased blood volume, amniotic fluid, and overall health. Drink plenty of water before, during, and after exercise.
- Wear Supportive Gear: Proper footwear and a supportive sports bra can help reduce discomfort and prevent injury.
- Mind Temperature: Avoid exercising in hot, humid weather. Choose a pleasant environment with proper ventilation and cooling options indoors.
- Balance Activity with Rest: While staying active is important, ensure to balance physical exertion with adequate rest to allow the body to recover and grow.
- Adapt Exercises in Later Trimesters: As the pregnancy progresses, modify activities to adapt to the shifting center of gravity and increase comfort and safety.
Incorporating physical activity into a pregnancy routine can significantly enhance health outcomes for both mother and child. By following expert recommendations and adapting exercises to suit personal capabilities, pregnant women can reduce the risk of gestational diabetes and enjoy a more comfortable, energetic pregnancy experience.