A Comprehensive Guide to Essential Vitamins and Supplements for Diabetics
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
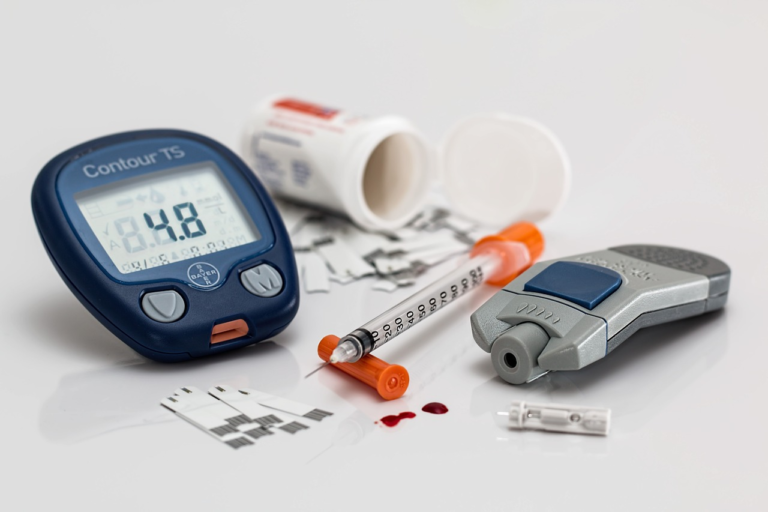
1. Introduction to Diabetes and Nutritional Needs
Diabetes is a chronic health condition that affects millions of people worldwide, encompassing several types, each with its own causes and implications. Understanding the different types of diabetes and the crucial role of nutrition in managing this condition is fundamental for those affected by it. In this introductory guide to diabetes and nutritional needs, we outline the types and prevalence of diabetes, highlight the importance of nutrition in its management, and explore the role of vitamins and supplements in supporting diabetic health.
Overview of Diabetes: Types and Prevalence
Diabetes is characterized by high levels of glucose in the blood due to impaired insulin production or function. There are primarily three types of diabetes:
- Type 1 Diabetes: An autoimmune condition where the body attacks and destroys insulin-producing beta cells in the pancreas. It typically manifests in childhood or early adulthood, although it can occur at any age. Type 1 diabetes accounts for about 5-10% of all diabetes cases.
- Type 2 Diabetes: The most common type, representing approximately 90-95% of diabetes cases. It usually develops in adults over the age of 45 but is increasingly seen in younger populations. Type 2 diabetes is often linked to obesity, inactivity, and genetic factors.
- Gestational Diabetes: This form occurs during pregnancy and typically resolves after childbirth. However, gestational diabetes increases the risk of developing type 2 diabetes later in life for both the mother and child.
The prevalence of diabetes is steadily increasing worldwide, with millions susceptible due to lifestyle factors and genetic predispositions. According to the International Diabetes Federation, it is estimated that over 500 million people will be living with diabetes by the year 2030.
Importance of Nutrition in Diabetes Management
Proper nutrition plays a pivotal role in managing diabetes. A well-balanced diet helps in maintaining blood glucose levels within target ranges, promoting overall health and preventing complications associated with diabetes. The following aspects highlight the importance of nutrition in diabetes management:
- Blood Sugar Control: Consuming a diet rich in complex carbohydrates, lean protein, and healthy fats can help regulate blood sugar levels.
- Weight Management: Maintaining a healthy weight is crucial for type 2 diabetes management and can help improve insulin sensitivity.
- Reduced Risk of Complications: A nutritious diet can lower the risk of complications such as heart disease, nerve damage, and kidney disease.
- Enhanced Energy Levels: Nutrient-rich foods provide sustained energy, helping manage fatigue—a common concern among diabetics.
Planning meals with a focus on portion control and understanding the glycemic index of foods are essential strategies for maintaining a balanced diet conducive to managing diabetes.
Role of Vitamins and Supplements in Supporting Diabetic Health
Vitamins and supplements can play a supportive role in managing diabetes, filling potential nutritional gaps and enhancing overall health. While a balanced diet is the primary method of obtaining necessary nutrients, certain vitamins and supplements may offer additional benefits:
- Vitamin D: Essential for bone health and immune function, vitamin D may improve insulin sensitivity and reduce inflammation.
- Omega-3 Fatty Acids: Found in fish oil, these can enhance heart health, a critical concern for individuals with diabetes.
- Magnesium: Adequate magnesium levels are essential for glucose metabolism and may reduce the risk of type 2 diabetes.
- Chromium: A trace mineral that may improve insulin action and lower blood glucose levels.
- Alpha-Lipoic Acid: An antioxidant linked to improved insulin sensitivity and neuropathy management.
It’s vital for individuals with diabetes to consult with healthcare providers before starting any vitamin or supplement regimen to ensure safety and efficacy, considering personal health needs and possible interactions with medications.
In conclusion, understanding the fundamental types and prevalence of diabetes, acknowledging the paramount importance of nutrition in managing this condition, and recognizing the supportive role vitamins and supplements can play is critical. For those living with diabetes, an integrative approach that combines medical treatment with optimized nutrition can significantly enhance quality of life and long-term health outcomes.

2. Key Vitamins for Diabetics
Managing diabetes effectively requires a comprehensive approach that includes a well-balanced diet rich in essential vitamins and nutrients. For diabetics, vitamins play a crucial role in maintaining overall health and mitigating the risks associated with the condition. In this guide, we will delve into the key vitamins for diabetics, focusing on Vitamin D, Vitamin B, and Vitamin C. Additionally, we’ll discuss how to choose the right vitamin sources and supplements.
Vitamin D: Benefits and Recommended Dosages
Vitamin D is a fat-soluble vitamin that is vital for maintaining healthy bones and supporting the immune system. For diabetics, Vitamin D offers several benefits:
- Improved Insulin Sensitivity: Research has shown that Vitamin D can enhance the body’s sensitivity to insulin, helping to better manage blood sugar levels.
- Bone Health: Diabetics are at a higher risk of bone fractures; Vitamin D’s role in calcium absorption contributes to stronger bones.
- Immune Support: Maintaining sufficient Vitamin D levels can help bolster the immune system, protecting against infections that diabetics are more prone to.
The recommended dosage of Vitamin D for diabetics can vary based on individual needs. It’s generally advised to aim for a daily intake of 600-800 IU, but it’s important to consult with a healthcare provider for personalized recommendations.
Vitamin B: Importance for Nerve Health and Energy Levels
Vitamin B is a complex of several essential nutrients that are crucial for maintaining nerve health and energy levels. This vitamin is especially important for diabetics:
- Nerve Health: Diabetics often suffer from neuropathy, a condition affecting nerve function. B vitamins, particularly B12, B6, and B1, are vital in protecting nerves and reducing symptoms.
- Energy Production: B vitamins play a critical role in converting food into energy, which is essential for managing fatigue commonly associated with diabetes.
- Cell Metabolism: These vitamins help in the formation of red blood cells and the proper functioning of the nervous system.
The recommended dosages of B vitamins can differ based on the specific type of B vitamin. For instance, Vitamin B12 is typically recommended at 2.4 mcg daily, while Vitamin B6 is suggested around 1.3-2 mg. Again, consulting with a healthcare provider for tailored advice is wise.
Vitamin C: Role in Reducing Inflammation and Boosting Immunity
Vitamin C, or ascorbic acid, is another crucial vitamin for diabetics. Its primary roles include:
- Inflammation Reduction: Chronic inflammation is a common issue in diabetics, and Vitamin C helps reduce oxidative stress and inflammation.
- Immune System Enhancement: As an antioxidant, Vitamin C supports the immune system, protecting against infections and promoting healing.
- Improved Glycemic Control: Some studies suggest that Vitamin C can help improve blood glucose levels, reducing the risk of complications.
A daily intake of 65-90 mg of Vitamin C is generally recommended. However, diabetics should discuss their specific needs with a healthcare provider to determine the appropriate dosage.
How to Choose the Right Vitamin Sources and Supplements for Diabetes
Choosing the right vitamin sources and supplements can help manage diabetes more effectively. Here’s a simple guide to making informed choices:
- Natural Food Sources:
- Include a variety of fruits and vegetables in your diet to boost your intake of essential vitamins.
- Incorporate fish, dairy, and fortified foods rich in Vitamin D.
- Opt for whole grains and lean meats to get sufficient B vitamins.
- Citrus fruits and berries are excellent sources of Vitamin C.
- Supplement Considerations:
- Consult with a healthcare provider before starting any supplements to cater to personal health conditions.
- Choose high-quality brands that offer transparency about their ingredients and nutrient levels.
- Monitor how your body responds to supplements and adjust as necessary.
- Assess Potential Interactions:
- Be mindful of how vitamin supplements might interact with your diabetes medication.
- Discuss all supplements and medications with your healthcare provider to avoid adverse interactions.
By focusing on a diet rich in these critical vitamins and choosing the right supplements, diabetics can improve their overall health, enhance immune function, and better manage their condition. Always consult with healthcare professionals to customize your vitamin intake according to individual health requirements.

3. Essential Minerals for Diabetes Management
Managing diabetes effectively involves not only monitoring blood sugar levels but also ensuring a proper intake of essential minerals that play critical roles in metabolic functions. These minerals, including magnesium, chromium, and zinc, influence various bodily processes that can aid in diabetes management. Understanding their benefits and incorporating them into a diabetic diet can lead to improved health outcomes. Here, we delve into the importance of these minerals and offer practical tips for integrating them into your nutritional regimen.
Magnesium: Impact on Insulin Sensitivity and Blood Sugar Levels
Magnesium is a crucial mineral that has a significant impact on insulin sensitivity and blood sugar control. It acts as a cofactor in over 300 enzymatic reactions, many of which are involved in glucose metabolism.
- Insulin Sensitivity: Magnesium helps to improve insulin sensitivity by facilitating insulin signal transmission. Studies suggest that higher magnesium intake is associated with lower fasting glucose levels and improved insulin response.
- Blood Sugar Levels: Adequate magnesium levels are linked to better control of blood sugar levels. Individuals with diabetes often have lower magnesium levels, and supplementation has been shown to improve HbA1c levels and insulin resistance.
Chromium: Regulation of Glucose and Lipid Metabolism
Chromium plays a pivotal role in regulating glucose metabolism and improving lipid profiles in individuals with diabetes. It enhances the action of insulin, the hormone critical for carbohydrate, fat, and protein metabolism.
- Glucose Metabolism: Chromium assists in moving glucose into cells by enhancing the activity of insulin. This effect helps keep blood sugar levels in check, particularly after meals.
- Lipid Metabolism: Adequate chromium levels can improve lipid profiles by reducing LDL cholesterol and increasing HDL cholesterol, which is beneficial for cardiovascular health.
Zinc: Enhancing Immune Function and Wound Healing
Zinc is essential for maintaining a strong immune system and promoting wound healing, both critical factors for individuals with diabetes who may experience impaired healing and a higher risk of infections.
- Immune Function: Zinc is vital for immune cell function and signaling. Adequate zinc levels can enhance the body’s defense mechanisms, reducing the risk of infections.
- Wound Healing: Zinc supports collagen synthesis and cell proliferation, necessary for repairing skin damage. It can accelerate wound healing, a crucial benefit for diabetic patients prone to skin ulcers and infections.
Tips for Incorporating Mineral-Rich Foods and Supplements into a Diabetic Diet
Incorporating foods rich in magnesium, chromium, and zinc can provide a natural source of these essential minerals. Here are some strategies to ensure you meet your dietary needs:
- Focus on Whole Foods:
- Introduce more leafy greens, nuts, seeds, and whole grains to boost magnesium intake.
- Include broccoli, grape juice, and whole-grain products for dietary chromium.
- Consume beans, nuts, and dairy products as excellent zinc sources.
- Consider Mineral Supplements:
If dietary changes are insufficient, consult with a healthcare provider about taking supplements. Choose high-quality products and follow the recommended dosages. - Maintain Balanced Nutrition:
Ensure your diet is well-rounded with a varied selection of fruits, vegetables, lean proteins, and healthy fats to support overall health and optimize minerals intake. - Monitor Blood Levels Regularly:
Regular blood tests can help track nutrient levels, ensuring that your dietary strategy is effective. Speak with your healthcare provider about adjusting your diet based on results.
Implementing these tips effectively into your daily routine can significantly impact diabetes management. By understanding the role of magnesium, chromium, and zinc, and strategically incorporating them into your diet, you support your body in managing diabetes more effectively.
4. Specialized Supplements that Aid Diabetes Control
Managing diabetes effectively often requires a full-spectrum approach that includes dietary management, medication, and lifestyle changes. While these components are crucial, specialized supplements can offer additional support by targeting specific complications associated with diabetes. This segment dives into the benefits and mechanisms of three key supplements: Omega-3 fatty acids, Alpha-lipoic acid, and Probiotics. It also evaluates the safety and efficacy of diabetes-specific supplements, helping individuals make informed choices.
Omega-3 Fatty Acids: Cardiovascular Benefits for Diabetics
Omega-3 fatty acids, primarily found in fish oils, are renowned for their cardiovascular benefits, which are particularly advantageous for people with diabetes. Diabetes significantly increases the risk of cardiac diseases, making heart health a priority.
- Anti-inflammatory Properties: Chronic inflammation is a common issue in diabetes. Omega-3 fatty acids like EPA and DHA have potent anti-inflammatory effects, which can help minimize vascular inflammation.
- Lipid Profile Improvement: Omega-3s may help in reducing triglycerides, a known risk factor for heart disease. Lowering triglycerides can subsequently mitigate cardiovascular risks.
- Blood Pressure Regulation: Regular intake of Omega-3 fatty acids has shown to assist in maintaining healthy blood pressure levels, thereby benefiting heart health.
Including a diet rich in Omega-3s or the use of supplements can thus support cardiovascular function in diabetics, reducing associated complications.
Alpha-Lipoic Acid: Protection Against Neuropathy and Oxidative Stress
Alpha-lipoic acid (ALA) is another vital supplement that comes into play with diabetes management due to its multifaceted benefits.
- Antioxidant Effects: As a powerful antioxidant, ALA helps neutralize free radicals, minimizing oxidative stress, a significant concern in diabetes.
- Neuroprotective Properties: ALA is well-regarded for its ability to alleviate symptoms of diabetic neuropathy, a common and painful complication.
- Insulin Sensitivity: Some studies suggest ALA may enhance insulin sensitivity, helping better manage blood glucose levels.
These attributes make Alpha-lipoic acid a supplementary choice to protect against nerve damage and oxidative stress in diabetic patients.
Probiotics: Role in Gut Health and Insulin Resistance
Probiotics, beneficial bacteria for the gut, have been increasingly recognized for their impact on overall health, particularly in managing insulin resistance, a hallmark of type 2 diabetes.
- Gut Microbiota Balance: Probiotics assist in maintaining a healthy gut microbiome, which is instrumental in regulating metabolic processes.
- Insulin Sensitivity Improvement: By modulating gut flora, probiotics can enhance insulin sensitivity, thereby aiding in more efficient glucose processing.
- Inflammation Reduction: Certain strains of probiotics can reduce systemic inflammation, a contributing factor to insulin resistance.
By promoting a balanced gut microbiome, probiotics can support and improve metabolic health, which is vital for diabetes management.
Evaluating the Safety and Efficacy of Diabetes-Specific Supplements
While supplements offer promising benefits, evaluating their safety and efficacy is crucial before incorporating them into a diabetes management plan. Here is a systematic approach to consider:
- Research-Based Evidence: Ensure there’s substantial scientific evidence supporting the supplement’s benefits. Clinical trials and studies are the gold standard.
- Consult with Healthcare Providers: It’s essential to discuss with a doctor or a certified nutritionist before starting any supplement, especially for individuals on medication.
- Check for Third-Party Testing: Opt for supplements that have been verified by third-party organizations for quality and purity to avoid adulterated products.
- Monitor for Side Effects: Be aware of any adverse effects and consult healthcare professionals if any arise.
- Adopt a Holistic Approach: Supplements should not replace prescribed medications or diabetic care routines but complement them.
By approaching supplements with careful consideration and expert guidance, individuals with diabetes can effectively utilize them as part of a comprehensive care strategy.
In conclusion, while specialized supplements such as Omega-3 fatty acids, Alpha-lipoic acid, and Probiotics present valuable benefits in managing diabetes, the key lies in informed and mindful integration into one’s lifestyle. Understanding their unique roles and ensuring their safe application pave the path toward improved health and quality of life for those managing diabetes.