Breaking Down The Link Between Polycystic Ovary Syndrome (PCOS) And Type Diabetes
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Polycystic Ovary Syndrome (PCOS) and Type Diabetes
Understanding the complexities of women’s health involves delving into various conditions that significantly impact their lives. Two of these conditions are Polycystic Ovary Syndrome (PCOS) and Type 2 Diabetes. While they may seem unrelated at first glance, emerging research suggests a connection between them that warrants exploration.
Understanding PCOS: Definition, Prevalence, and Symptoms
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder common among women of reproductive age. It is characterized by irregular menstrual cycles, excess androgen levels, and polycystic ovaries. Understanding the different aspects of this condition is crucial for better management and mitigation of its effects.
- Definition: PCOS is a syndrome affecting the endocrine system, leading to an imbalance of female sex hormones.
- Prevalence: It affects approximately 5-10% of women worldwide, making it one of the most common hormonal disorders in females.
- Symptoms: The symptoms vary but commonly include:
- Irregular periods or no periods at all.
- Excessive hair growth (hirsutism) predominantly on the face, chest, and back.
- Weight gain and difficulty losing weight.
- Oily skin or acne.
- Thinning hair or male-pattern baldness.
The impacts of PCOS extend beyond these immediate symptoms. Women with PCOS often deal with multiple long-term health challenges, including infertility and metabolic syndrome, which comprises obesity, high blood pressure, high blood sugar levels, and abnormal cholesterol levels.
Overview of Type 2 Diabetes: Causes, Symptoms, and Risk Factors
Type 2 Diabetes is a chronic condition that affects the way the body processes blood sugar (glucose). It is characterized by insulin resistance, where the body doesn’t use insulin properly, leading to elevated blood glucose levels. Here’s a brief overview:
- Causes: While the precise cause of Type 2 Diabetes is not fully understood, several factors contribute to its development:
- Genetic predisposition: Having a family history of diabetes can increase the risk.
- Lifestyle factors: Poor diet, physical inactivity, and obesity are significant contributors.
- Insulin resistance: The body’s cells become resistant to insulin, leading to high blood sugar levels.
- Symptoms: Symptoms of Type 2 Diabetes often develop slowly and may include:
- Increased thirst and frequent urination.
- Extreme hunger.
- Unintended weight loss.
- Fatigue and weakness.
- Blurred vision.
- Slow-healing sores or frequent infections.
- Risk Factors: Some factors increase the likelihood of developing Type 2 Diabetes, including:
- Age: The risk increases significantly after age 45.
- Weight: Being overweight is a primary risk factor.
- Physical inactivity: Leading a sedentary lifestyle contributes to the condition.
- Ethnicity: Certain ethnicities, such as African-Americans, Hispanics, and South Asians, are at higher risk.
Type 2 Diabetes is a significant public health concern due to its increasing prevalence and the complications it can lead to, such as heart disease, nerve damage, kidney damage, and vision problems.
Explanation of the Need to Explore the Connection between PCOS and Type 2 Diabetes
With both PCOS and Type 2 Diabetes posing significant challenges in their own right, it is crucial to understand the intricate relationship between these two conditions.
- Shared Pathophysiology: Both conditions exhibit insulin resistance, which is a potential link between them.
- Increased Risk: Women with PCOS are at a higher risk of developing Type 2 Diabetes due to overlapping risk factors such as obesity and insulin resistance.
- Hormonal Influence: Hormonal imbalances in PCOS may exacerbate metabolic disturbances, contributing to diabetes risk.
- Comprehensive Management: Understanding the connection allows for more effective management strategies that address both conditions simultaneously.
Addressing this link is vital for healthcare providers to improve the quality of life for women with PCOS, offering early interventions that could prevent or delay the onset of Type 2 Diabetes.
In conclusion, by understanding the nuances of PCOS and Type 2 Diabetes, medical researchers can continue to investigate their connection, paving the way for innovative treatments and preventive measures. This exploration is not just a scientific inquiry but a necessary step toward enhancing women’s health globally.

2. Pathophysiological Connection between PCOS and Type Diabetes
Pathophysiological Connection between PCOS and Type 2 Diabetes
Polycystic Ovary Syndrome (PCOS) and Type 2 Diabetes are interconnected medical conditions associated with insulin resistance, hormonal imbalances, and various genetic and environmental factors. Understanding the pathophysiological relationship between these two conditions is crucial for improving diagnosis, treatment, and management. Below, we delve deeper into these intricate connections, elucidating how they contribute to the development of each condition.
-
Insulin Resistance: A Common Link between PCOS and Type 2 Diabetes
Insulin resistance is recognized as a pivotal factor that connects PCOS and Type 2 Diabetes. This condition occurs when cells in the body become less responsive to insulin, leading to elevated blood glucose levels. Below, we explore how insulin resistance serves as a link between these two conditions:
-
PCOS and Insulin Resistance:
In many women with PCOS, insulin resistance is a prevalent feature. This resistance contributes to hyperinsulinemia, which exacerbates ovarian dysfunction, leading to irregular menstrual cycles and anovulation.
-
Type 2 Diabetes and Insulin Resistance:
Insulin resistance is a hallmark of Type 2 Diabetes, resulting in difficulty maintaining normal blood glucose levels. Persistent insulin resistance eventually impairs pancreatic beta-cell function, precipitating diabetes.
-
Interconnection:
The presence of insulin resistance in both conditions suggests a common underlying pathophysiological mechanism, enhancing the risk of developing one condition in the presence of the other.
-
PCOS and Insulin Resistance:
-
Hormonal Imbalances: How They Contribute to Both Conditions
Hormonal imbalances constitute another shared feature between PCOS and Type 2 Diabetes. These imbalances involve various hormones, significantly impacting the development and progression of each condition:
-
PCOS and Hormonal Imbalances:
Women with PCOS often exhibit elevated androgen levels, contributing to symptoms such as hirsutism and acne. Additionally, imbalances in luteinizing hormone (LH) and follicle-stimulating hormone (FSH) affect ovarian function.
-
Diabetes and Hormonal Imbalances:
Type 2 Diabetes can lead to altered levels of insulin and glucagon. Moreover, chronic hyperglycemia may influence sex hormone-binding globulin (SHBG) levels, further complicating hormonal regulation.
-
Shared Pathways:
Insulin resistance may influence androgen production and SHBG levels, integrating hormonal imbalances as a shared pathway linking both conditions.
-
PCOS and Hormonal Imbalances:
-
Genetic and Environmental Factors: Contributions to Developing PCOS and Diabetes
A range of genetic and environmental factors influences the risk of developing both PCOS and Type 2 Diabetes. Understanding these factors provides insight into the etiology and potential preventative strategies:
-
Genetic Predisposition:
Genetic studies have identified several loci associated with both PCOS and Type 2 Diabetes, suggesting that shared genetic predispositions may exist. Family history is a significant risk factor for both conditions.
-
Environmental Influences:
Lifestyle factors, such as poor diet, sedentary behavior, and obesity, are known contributors to insulin resistance and both conditions. These factors often intersect with genetic predispositions, amplifying risk.
-
Integrative Approach:
An integrative approach that considers genetic vulnerabilities alongside lifestyle modifications is crucial for effective prevention and management strategies.
-
Genetic Predisposition:
In summary, the pathophysiological connection between PCOS and Type 2 Diabetes is multifaceted, involving insulin resistance, hormonal imbalances, and genetic and environmental factors. By gaining a deeper understanding of these interconnected mechanisms, healthcare providers can enhance diagnostic accuracy and develop targeted interventions that address the shared and distinct aspects of both conditions.

3. Risk Factors and Complications of PCOS Leading to Type Diabetes
Risk Factors and Complications of PCOS Leading to Type 2 Diabetes
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder affecting women of reproductive age. One of the most significant concerns associated with PCOS is its link to Type 2 Diabetes. This connection is primarily attributed to insulin resistance, a common feature of PCOS, which can eventually lead to the onset of diabetes. Understanding the risk factors and potential complications can help in taking proactive measures to manage these conditions effectively.
- Insulin Resistance: Women with PCOS often exhibit insulin resistance, which means their bodies are less responsive to insulin, resulting in higher blood glucose levels. This condition is a precursor to Type 2 Diabetes.
- Obesity: A significant number of women with PCOS struggle with obesity, which can further exacerbate insulin resistance and increase the risk of developing diabetes.
- Genetic Predisposition: Family history of Type 2 Diabetes can increase the likelihood of PCOS patients developing the disorder.
- Hormonal Imbalance: The hormonal imbalances in PCOS, particularly elevated levels of androgens, can contribute to insulin resistance.
Obesity and Weight Management: Impact on PCOS and Type 2 Diabetes
Obesity plays a critical role in the development and progression of both PCOS and Type 2 Diabetes. Effectively managing weight through strategic interventions can considerably alleviate symptoms and reduce risks.
- Body Mass Index (BMI) and PCOS: Women with higher BMIs are more susceptible to severe PCOS symptoms and are at an increased risk of developing Type 2 Diabetes. Weight loss, even modest, can improve insulin sensitivity and regularize menstrual cycles.
- Impact of Weight Loss: Losing weight can help lower insulin levels, reduce androgen levels, and restore ovulation, which is beneficial for managing both PCOS and the potential onset of Type 2 Diabetes.
- Effective Weight Management Strategies:
- Implementing balanced, nutritious meals to create a calorie deficit.
- Incorporating physical exercises, such as aerobic and resistance training.
- Seeking professional guidance from nutritionists and healthcare providers.
Lifestyle Factors: Diet, Physical Activity, and Their Influence
Lifestyle choices, particularly diet and physical activity, play a pivotal role in managing PCOS and mitigating the risk of Type 2 Diabetes. Emphasizing tailored lifestyle interventions can significantly enhance outcomes.
- Dietary Considerations:
- Low-Glycemic Index Diet: Foods with low glycemic index can help manage blood sugar levels effectively.
- High-Fiber Intake: Foods rich in fiber can improve insulin sensitivity and help manage weight.
- Avoiding Processed Foods: Reducing consumption of processed foods, which are often high in sugar and unhealthy fats, can prevent insulin spikes.
- Balanced Nutrient Intake: Ensuring a balance of proteins, healthy fats, and complex carbohydrates to maintain hormonal balance and energy levels.
- Physical Activity:
- Aerobic Exercise: Activities such as walking, cycling, or swimming improve cardiovascular health and aid in weight management.
- Resistance Training: Helps in building muscle mass, improving resting metabolic rate, and enhancing insulin sensitivity.
- Consistency: Regular physical activity, adapted to one’s capacity, ensures sustained benefits.
Long-term Health Risks: Cardiovascular Disease and Metabolic Syndrome
Women with PCOS are not only at an increased risk of developing Type 2 Diabetes but also face potential long-term health risks such as cardiovascular disease and metabolic syndrome. Identifying these risks early and implementing strategic interventions is crucial for long-term health.
- Cardiovascular Disease Risk: Due to factors such as insulin resistance, obesity, and hypertension, women with PCOS have a heightened risk of heart disease. Monitoring and managing blood cholesterol, blood sugar, and blood pressure levels are vital.
- Metabolic Syndrome: PCOS is often associated with components of metabolic syndrome, including abdominal obesity, dyslipidemia, and hypertension. These factors, combined, significantly increase the risk of cardiovascular ailments.
- Preventive Measures:
- Regular health screenings to monitor risk factors.
- Adopting heart-healthy diets rich in omega-3 fatty acids, antioxidants, and fiber.
- Maintaining a consistent exercise routine to support cardiovascular health and metabolic functions.
- Collaborating with healthcare providers for personalized medical interventions.
In summary, understanding the intricate relationship between PCOS and Type 2 Diabetes is essential for managing both conditions effectively. By addressing weight management, optimizing lifestyle factors such as diet and exercise, and being vigilant about long-term health risks, women with PCOS can significantly enhance their health outcomes and reduce the likelihood of developing diabetes and associated complications.
4. Diagnostic Approaches and Managing PCOS in Relation to Type Diabetes
Polycystic Ovary Syndrome (PCOS) and type 2 diabetes are interrelated metabolic disorders that require comprehensive diagnostic and management strategies. Both conditions share common pathophysiological mechanisms which often complicate their diagnosis and treatment. Understanding the diagnostic criteria and medical assessments for these conditions is paramount for clinicians. Furthermore, exploring effective treatment strategies such as medications, lifestyle changes, and other medical interventions is crucial to managing these conditions effectively. The role of healthcare providers in coordinating care is also fundamental in ensuring optimal patient outcomes.
Diagnostic Criteria and Medical Assessments: For PCOS and Diabetes
The diagnosis of PCOS and type 2 diabetes involves a series of clinical criteria and assessments to accurately identify and differentiate the conditions. It’s essential to diagnose these conditions early to prevent complications and guide appropriate treatment.
Diagnostic Criteria for PCOS
- Hyperandrogenism: Clinical signs such as hirsutism, acne, and male-pattern baldness, or elevated androgen levels detected through blood tests.
- Oligo-ovulation or Anovulation: Irregular or absent menstrual cycles, indicating disrupted ovulation.
- Polycystic Ovaries: Identified through ultrasound, showing enlarged ovaries with multiple small follicles or cysts.
It is important to note that other conditions such as thyroid dysfunction and hyperprolactinemia should be excluded before confirming a diagnosis of PCOS. The presence of at least two of the above criteria is generally required according to common diagnostic guidelines such as the Rotterdam criteria.
Diagnostic Criteria for Type 2 Diabetes
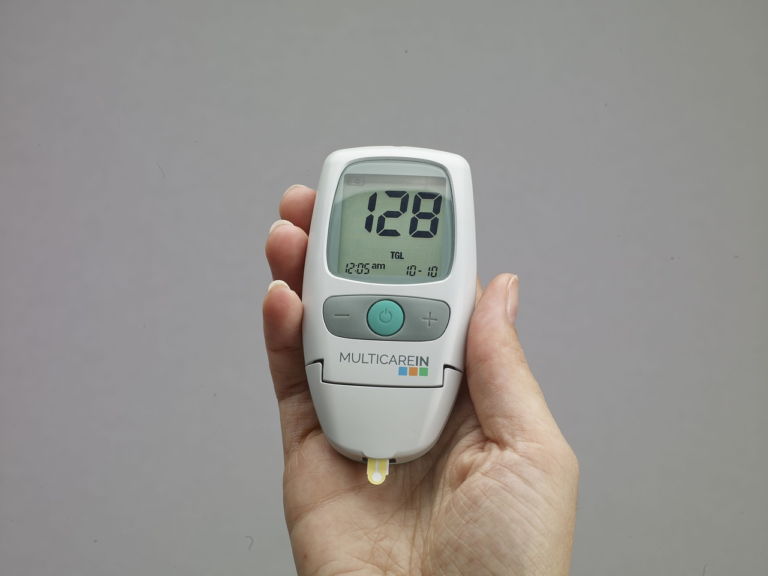
- Fasting Plasma Glucose Test: A fasting glucose level of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes.
- Glycated Hemoglobin (A1C) Test: An A1C level of 6.5% (48 mmol/mol) or higher suggests diabetes.
- Oral Glucose Tolerance Test (OGTT): A 2-hour plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher, 2 hours after drinking a glucose beverage, confirms diabetes.
In cases where results are borderline, it may be necessary to repeat tests to confirm the diagnosis, especially when there are risk factors or symptoms present.
Treatment Strategies: Medications, Lifestyle Changes, and Medical Interventions
Treating PCOS and type 2 diabetes necessitates a multifaceted approach that includes medication, lifestyle modifications, and potentially other medical interventions. Personalized treatment plans are essential since both conditions share insulin resistance as a common thread.
Medications
- Metformin: Frequently used for both PCOS and type 2 diabetes, metformin helps improve insulin sensitivity and can aid in ovulation regulation for women with PCOS.
- Hormonal Contraceptives: In women with PCOS, oral contraceptives may be used to regulate menstrual cycles, reduce androgen levels, and alleviate symptoms such as acne and hirsutism.
- Insulin Therapy: Necessary for managing blood glucose levels in patients with type 2 diabetes, particularly when other medications are insufficient.
Lifestyle Changes
- Diet: A balanced diet rich in whole grains, fruits, and vegetables, low in refined carbohydrates and sugars, is essential for managing both conditions. Monitoring carbohydrate intake can aid in blood glucose control.
- Exercise: Regular physical activity improves insulin sensitivity and assists with weight management. Activities such as brisk walking, swimming, or cycling are beneficial.
- Weight Management: Achieving a healthy weight can significantly improve symptoms of PCOS and enhance glycemic control in diabetes. Even modest weight loss can have a positive impact.
Medical Interventions
- Ovarian Drilling: In certain cases of PCOS where other treatments fail, laparoscopic ovarian drilling may be recommended to induce ovulation.
- Bariatric Surgery: For patients with severe obesity and uncontrollable diabetes, surgical interventions might be considered to improve long-term health outcomes.
Role of Healthcare Providers: Coordinating Care to Manage Both Conditions
Effective management of PCOS and type 2 diabetes heavily relies on the coordinated efforts of a multidisciplinary healthcare team. These professionals offer expertise and guidance tailored to the unique needs of each individual.
Coordinating Care
- Primary Care Physician: The first point of contact who coordinates overall patient care, including routine screenings and referrals to specialists as necessary.
- Endocrinologist: Specializes in hormonal disorders and metabolism, providing targeted medical management for both PCOS and diabetes.
- Gynecologist: Focuses on reproductive health and guides treatment specifically related to PCOS’s effects on the menstrual cycle and fertility.
Collaboration among these providers promotes a comprehensive and cohesive treatment plan, ensuring all aspects of the patient’s health are monitored and optimized for the best possible outcomes.
In conclusion, managing PCOS and type 2 diabetes requires an integrated approach involving precise diagnostic evaluations, effective medication and lifestyle management strategies, and synchronized efforts from healthcare professionals. By understanding the intricate relationship between these conditions and utilizing a multidisciplinary care model, patients can achieve improved health and quality of life.