Understanding The Connection Between Depression And diabetes – Tips For Coping With Both Conditions
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to the Link Between Depression and Diabetes
Both depression and diabetes are among the most prevalent health issues facing modern society, each posing significant challenges on their own. However, the intersection of these two conditions is particularly concerning, as they often co-occur and can exacerbate one another. Understanding the relationship between depression and diabetes is crucial for patients, healthcare providers, and policymakers alike.
To kick off this exploration, it’s essential to grasp the individual characteristics and implications of depression and diabetes as separate maladies.
- Depression: Depression is a mental health disorder characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in daily activities. Individuals with depression may also experience changes in appetite, sleep disturbances, fatigue, and difficulty concentrating. The exact cause of depression is unknown, but it is believed to result from a combination of genetic, biological, environmental, and psychological factors.
- Diabetes: Diabetes is a chronic physical condition affecting how the body processes blood sugar (glucose). The two primary forms of diabetes are Type 1 and Type 2. Type 1 diabetes is an autoimmune condition where the body’s immune system attacks insulin-producing cells, while Type 2 diabetes involves the body becoming resistant to insulin. Symptoms include increased thirst, frequent urination, extreme fatigue, and blurred vision. Without proper management, diabetes can lead to significant health complications.
Given these brief overviews, it becomes essential to discuss the underlying connection between mental health disorders like depression and chronic physical illnesses such as diabetes.
Connection Between Mental Health and Chronic Physical Illnesses
Chronic physical illnesses and mental health conditions are intricately connected. Mental health significantly affects the development, course, and outcome of chronic illnesses. Conversely, chronic diseases can lead to mental health challenges for individuals.
- Psychological stress and biological changes due to chronic conditions can influence mental health status.
- The self-management requirements of chronic illnesses often lead to emotional stress and mental health dilemmas such as anxiety and depression.
- Conversely, depression can impair a person’s ability to manage their diabetes effectively, adhering to dietary restrictions, exercise, and medication regimes.
Furthermore, some research suggests that inflammation, hormonal imbalances, and neuroendocrine changes may work as mechanisms intertwining these conditions, illustrating a bidirectional relationship.
Statistics of Coexisting Depression and Diabetes
Research and statistics consistently demonstrate that people with diabetes face a higher risk of developing depression compared to the general population. The coexistence of these conditions poses complex treatment challenges and increases the overall burden on healthcare systems globally.
Here are some pivotal statistics reflecting the prevalence of coexisting depression and diabetes:
- A meta-analysis published in the Journal of Affective Disorders reported that depression is present in 19% of people with Type 1 diabetes and 25% of those with Type 2 diabetes.
- According to the American Diabetes Association, the prevalence of major depression in individuals with diabetes is approximately two-fold higher compared to those without diabetes.
- The Centers for Disease Control and Prevention (CDC) highlights that people with diabetes are 2 to 3 times more likely to have depression than people without diabetes.
- A longitudinal study published in Diabetes Care found that depression occurs in 15% of patients before being diagnosed with diabetes, indicating potential causation or a common pathophysiology.
These statistics emphasize the pressing need for integrated healthcare approaches focusing on both mental and physical health. Addressing this dual challenge requires multi-disciplinary collaboration and a holistic understanding of how psychological and physiological pathways intertwine in chronic illnesses.
Thus, the link between depression and diabetes is a pertinent issue that demands further exploration and awareness within the medical community and society at large. Understanding this connection is indispensable for the development of preventative measures, early detection, and effective treatment strategies.

2. How Depression Can Impact Diabetes Management
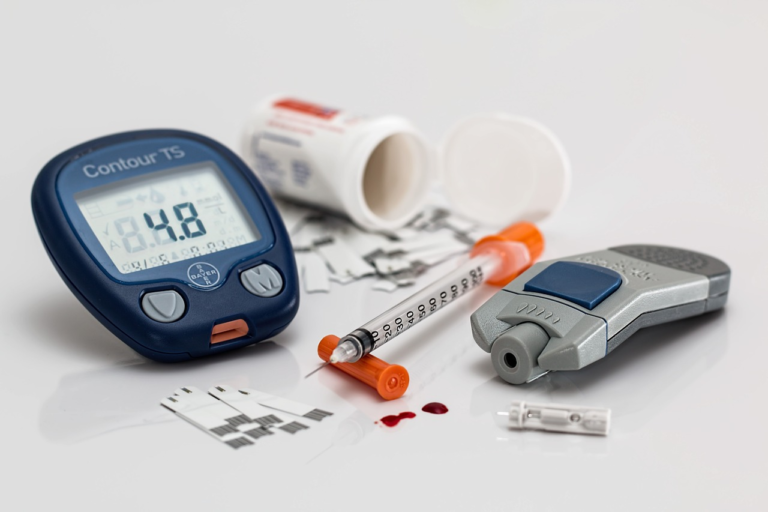
Dealing with diabetes is a lifelong commitment that requires continuous monitoring of blood sugar levels, adherence to medications, regular physical activity, and appropriate dietary choices. When depression enters the picture, these self-care behaviors can be severely affected, leading to a vicious cycle where each condition worsens the other.
How Depressive Symptoms Can Hinder Diabetes Self-Care Behaviors
Depression is characterized by persistent feelings of sadness, hopelessness, and lack of interest in daily activities. These symptoms can significantly interfere with the management of diabetes in several ways:
- Lack of Motivation: Individuals with depression often struggle with severe fatigue and apathy, making it difficult to perform necessary daily diabetes management tasks such as blood glucose monitoring and maintaining a healthy diet.
- Cognitive Impairment: Depression can lead to cognitive issues such as poor concentration, memory problems, and indecisiveness. These impairments can lead to forgetfulness in taking medications or attending medical appointments.
- Emotional Eating: Those who experience depressive symptoms may turn to food for comfort, especially high-calorie and high-sugar foods, which can disrupt blood sugar levels.
Collectively, these challenges can lead to inadequate diabetes control, ultimately worsening both depression and diabetes simultaneously.
Overview of Potential Complications Arising from Lack of Diabetes Control Due to Mental Health Issues
When diabetes is not properly managed due to the impact of depressive symptoms, it can lead to a range of serious complications. Here are some potential health consequences:
- Cardiovascular Problems: Poorly managed diabetes increases the risk of high blood pressure, heart disease, and stroke. Depression adds to this risk by affecting lifestyle choices and metabolic health.
- Nerve Damage (Neuropathy): Uncontrolled blood sugar levels can cause nerve damage throughout the body, leading to pain, numbness, and even digestive issues.
- Kidney Damage (Nephropathy): High blood sugar can damage the kidneys over time, leading to kidney disease or failure.
Each of these conditions can be exacerbated by the presence of depression, creating a compounding effect that makes treatment more challenging.
The Psychological Stress of Diabetes as a Potential Trigger for Depression
The constant vigilance and lifestyle alterations required to manage diabetes can become a significant psychological burden, contributing to the onset of depression in some individuals:
- Chronic Stress: The ongoing stress of managing blood sugar levels, dealing with potential complications, and maintaining a balanced lifestyle can exhaust a person’s mental resources, potentially leading to depression.
- Stigma and Social Isolation: Experiencing shame or stigma associated with diabetes can lead to social withdrawal and feelings of isolation, both of which are known factors in developing depression.
- Disappointment and Frustration: Setbacks in managing diabetes or dealing with frequent health crises can lead to feelings of inadequacy and frustration, further exacerbating depressive symptoms.
Understanding this bidirectional relationship between diabetes and depression is crucial for healthcare providers to offer comprehensive care that addresses both physical and mental health needs.
In conclusion, the interplay between depression and diabetes management emphasizes the need for integrated healthcare approaches. It is essential to address mental health proactively to facilitate better physical health outcomes for individuals with diabetes.

3. Recognizing the Signs and Symptoms of Coexisting Depression and Diabetes
Recognizing the signs and symptoms of coexisting depression and diabetes is crucial in managing both conditions effectively. While both diseases have distinct characteristics, they often exhibit overlapping symptoms that can complicate diagnosis and treatment.
Common Symptoms of Depression and Diabetes That Overlap
Both depression and diabetes are prevalent chronic conditions that can significantly impact a person’s quality of life. Understanding their overlapping symptoms is a vital step in ensuring proper care and management. Symptoms that might be seen in both conditions include:
- Fatigue: Chronic tiredness is commonly reported by patients with depression and diabetes. While depression can make individuals feel perpetually exhausted, diabetes-related fatigue might result from fluctuating blood sugar levels.
- Changes in Appetite: Both conditions can cause fluctuations in appetite. Depression might lead to increased or decreased eating as a form of coping, while diabetes can prompt appetite changes due to blood sugar imbalances.
- Weight Fluctuations: Weight gain or loss may occur. In depression, weight changes are often linked to changes in appetite and lifestyle. In diabetes, they can be related to improper blood sugar control.
- Difficulty Concentrating: Both conditions can decrease mental clarity and the ability to concentrate, partly due to fatigue and partly due to the brain chemistry changes associated with each condition.
- Sleep Disturbances: Individuals may experience insomnia or hypersomnia. Depression can disrupt sleep patterns, while diabetes may affect sleep through nocturia or neuropathy.
How to Differentiate Between Physical Symptoms of Diabetes and Symptoms of Depression
Differentiating between the symptoms of diabetes and depression requires a nuanced understanding of both conditions. While there are overlaps, certain characteristics can help in distinguishing between the two. Consider the following aspects:
- Blood Sugar Monitoring: Regular testing can help determine if fatigue or mood changes are related to blood sugar levels, suggesting that diabetes is the primary cause.
- Psychological Evaluation: A mental health professional can assess symptoms within the framework of mood disorders, offering a clearer perspective on whether depression is the underlying cause.
- Contextual Analysis: Evaluate whether symptoms are situational (more likely to be depression-related) or correlate with changes in blood sugar readings (more likely to be related to diabetes).
- Duration of Symptoms: Chronic hyperglycemia symptoms might manifest differently over time compared to persistent depressive symptoms, which are typically continuous and not contingent on diet or lifestyle.
Importance of Early Diagnosis and Intervention in Both Conditions
Early diagnosis and intervention in depression and diabetes are critical for several reasons:
- Comprehensive Management: Addressing both conditions simultaneously ensures that the treatment plan is holistic and considers the interaction between psychological and physiological health.
- Improved Prognosis: Early intervention can lead to better long-term health outcomes, reducing the risk of complications associated with both depression and diabetes.
- Quality of Life: Timely treatment can significantly enhance the individual’s quality of life, addressing symptoms before they worsen and addressing comorbidities effectively.
- Reduction of Healthcare Costs: Detecting and managing these conditions early can reduce the need for long-term medical treatments and hospitalizations, leading to lower healthcare costs.
To conclude, recognizing and distinguishing the signs and symptoms of coexisting depression and diabetes is paramount. By acknowledging their overlap, employing precise diagnostic methods, and pursuing early treatment, individuals can achieve better health outcomes and lead more fulfilling lives.
4. Effective Strategies for Coping with Depression and Diabetes
Managing both depression and diabetes can be challenging, but implementing effective strategies can significantly improve your quality of life. This involves integrating lifestyle changes, therapy, and support systems. Let’s explore these strategies in detail.
Lifestyle Changes That Benefit Both Mental Health and Diabetes Management
Adopting a healthy lifestyle is crucial for managing both depression and diabetes. Here are some beneficial changes you can make:
-
Diet:
Eating a balanced diet is essential. Focus on whole grains, lean proteins, and plenty of fruits and vegetables. These foods stabilize blood sugar levels and enhance mood by providing the necessary nutrients to optimize brain function.
Limit your intake of refined sugars and carbohydrates, as they can cause fluctuations in blood sugar levels, leading to mood swings. Incorporating omega-3 fatty acids, found in fish like salmon and mackerel, can further support mental health!
-
Exercise:
Regular physical activity is a powerful tool for managing both conditions. Aim for at least 150 minutes of moderate exercise per week, such as walking, swimming, or cycling. Exercise helps regulate blood sugar levels, improve cardiovascular health, and release endorphins, which act as natural mood lifters.
-
Sleep:
Quality sleep is vital. Aim for 7-9 hours each night to help regulate mood and maintain proper glucose metabolism. Establish a relaxing bedtime routine and create a sleep-friendly environment to enhance sleep quality.
The Role of Therapy and Counseling in Managing Depression and Diabetes
Seeking therapy can be a transformative step in managing both depression and diabetes. Cognitive-behavioral therapy (CBT) is particularly effective.
-
Cognitive-Behavioral Therapy (CBT):
CBT focuses on identifying and changing negative thought patterns and behaviors. It has been proven to reduce symptoms of depression while helping individuals develop effective strategies for managing diabetes.
Engaging with a trained therapist allows you to set realistic goals, develop problem-solving skills, and promote a more positive outlook on life.
-
Other Therapeutic Approaches:
Aside from CBT, other therapeutic methods like mindfulness-based therapy and acceptance and commitment therapy (ACT) can also be beneficial. These approaches help individuals embrace their experiences, reduce stress, and foster a positive mental state.
Importance of Support Systems
Support from family, friends, and support groups functions as a cornerstone for managing both depression and diabetes. These networks provide motivation, encouragement, and practical advice.
-
Family and Friends:
Open communication with family and friends about your struggles can foster understanding and provide emotional support. They can help you stick to your healthy lifestyle choices and offer companionship to reduce the feelings of isolation and loneliness often associated with depression.
-
Support Groups:
Joining support groups, either locally or online, connects you with individuals facing similar challenges.
- Sharing experiences and strategies offers practical insights.
- Witnessing others’ successes can serve as powerful motivation.
- Receiving empathetic support from peers who truly understand your situation.
-
Healthcare Providers:
Regular check-ins with healthcare providers ensure a comprehensive approach to managing both conditions. They can monitor your progress, adjust treatment plans, and offer referrals to specialists if necessary.
Combining lifestyle changes, therapy, and strong support systems creates a holistic approach to managing both depression and diabetes. Adopting these strategies not only helps balance physical and mental health but also enhances overall well-being, allowing you to lead a fulfilling and healthier life.