The Importance of Self-Care Practices for Those with Chronic Illnesses like Diabetes
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Self
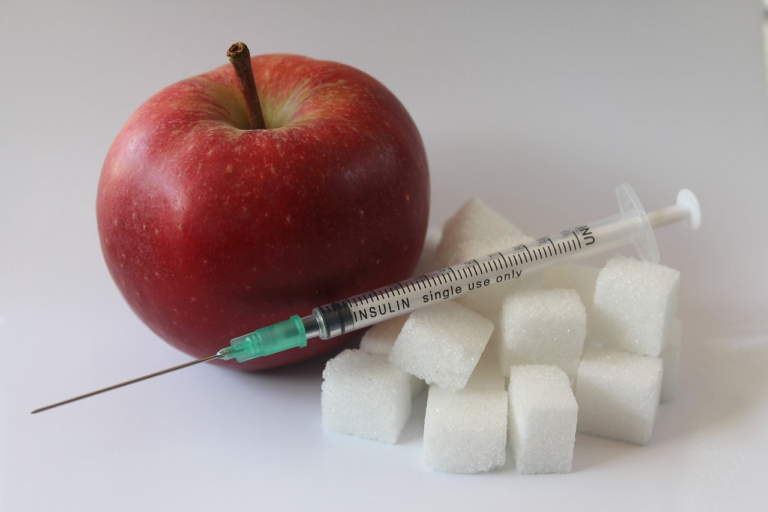
Chronic illnesses are a significant concern that impacts millions of individuals worldwide, influencing various aspects of daily life and overall well-being. Among these, diabetes stands out as one of the most common yet complex conditions that can have profound effects on both physical and mental health.
In essence, chronic illnesses refer to a group of long-lasting health conditions that often require ongoing medical attention and can limit daily activities. These diseases, by their nature, tend to persist over time, unlike acute conditions that resolve swiftly. They encompass a wide range of ailments, including heart disease, cancer, and arthritis, but for the purpose of this discussion, the focus will primarily be on diabetes.
- Diabetes: This chronic illness revolves around challenges in the body’s ability to process blood glucose, resulting either from the immune system attacking insulin-producing cells in Type 1 diabetes or from insulin resistance and deficiency in Type 2 diabetes. The complexity of diabetes requires individuals to engage in continuous management to prevent severe complications.
Given the lifelong journey that chronic illnesses such as diabetes entail, self-care emerges as a vital component in the management and improvement of life quality for individuals dealing with these conditions.
Self-care is defined as the actions individuals take to maintain health, prevent disease, and cope with illness without professional help. It is a concept that empowers individuals to make informed decisions regarding their health by engaging in daily activities and practices that promote physical and mental well-being.
The significance of self-care in the context of chronic illnesses cannot be overstated. It serves not only as a means to enhance the quality of life but also as a pivotal strategy in chronic disease management. For patients with diabetes, practicing self-care might include actively monitoring blood sugar levels, adhering to prescribed medication regimens, maintaining a balanced diet, and engaging in regular physical activity.
- Monitoring blood sugar levels
- Adhering to prescribed medication
- Maintaining a nutritious diet
- Engaging in physical activity
All these actions cumulatively contribute to better management of diabetes and other chronic diseases, allowing individuals to maintain more control over their health outcomes.
Thesis statement: Self-care plays an essential role in managing chronic illnesses, particularly diabetes, by empowering individuals to take control of their health and make proactive decisions that lead to improved well-being and enhanced quality of life.
Through fostering habits that prioritize health, well-being, and preventive care, self-care serves as a cornerstone in the journey of managing chronic illnesses effectively. It not only aids in symptom management but also mitigates the progression of ailments, preventing further complications. Chronic disease self-management is about understanding the illness, recognizing its symptoms, and knowing how to respond to such symptoms without relying predominantly on healthcare providers.
In conclusion, the integration of self-care into the routine management of chronic illnesses, especially diabetes, highlights a comprehensive approach to health that empowers patients to lead a fulfilling and balanced life under the constraints of their condition. Emphasizing holistic practices that involve physical, emotional, and psychological care, individuals with chronic diseases can navigate the complexities of their health challenges with resilience and confidence.

2. Understanding Chronic Illnesses: Focus on Diabetes
Understanding Chronic Illnesses: Focus on Diabetes
Diabetes is a chronic illness that has become a significant global health concern. Characterized by elevated blood glucose levels, diabetes occurs when the body is either unable to produce sufficient insulin or cannot effectively use the insulin it produces. This persistent condition requires ongoing medical attention and self-management to prevent acute complications and reduce the risk of long-term complications.
Explanation of Diabetes and Its Various Types
Diabetes is categorized into different types, each with unique characteristics and causes:
- Type 1 Diabetes: Often diagnosed in children and young adults, Type 1 diabetes is an autoimmune condition where the body’s immune system attacks insulin-producing cells in the pancreas. This results in little to no insulin production, necessitating lifelong insulin therapy. Understanding the early symptoms and the need for constant blood sugar monitoring is critical for managing Type 1 diabetes effectively.
- Type 2 Diabetes: This is the most common form of diabetes, typically occurring in adults. It arises when the body’s cells become resistant to insulin or the pancreas does not produce enough insulin. Lifestyle factors, such as obesity and physical inactivity, significantly increase the risk of developing Type 2 diabetes. Early intervention through diet, exercise, and medication can control blood sugar levels effectively.
- Gestational Diabetes: This type of diabetes is diagnosed during pregnancy and can pose risks to both mother and child if left unmanaged. Although gestational diabetes usually resolves after childbirth, it increases the risk of type 2 diabetes later in life for the mother.
- Other Specific Types: There are other less common types of diabetes that may result from specific genetic conditions, surgeries, medications, or other illnesses. Each type requires targeted treatment and management strategies.
Common Challenges Faced by Individuals with Diabetes
Living with diabetes presents various challenges that impact day-to-day life:
- Blood Sugar Management: Individuals with diabetes must regularly monitor their blood glucose levels. This requires frequent testing, careful meal planning, and medication or insulin administration. Balancing these factors to maintain optimal blood sugar levels can be a constant struggle.
- Dietary Restrictions: Adhering to specific dietary guidelines is vital for managing diabetes. This includes controlling carbohydrate intake and being mindful of nutritional labels, which can be challenging in social settings or when dining out.
- Emotional and Mental Health: Managing a chronic illness like diabetes can lead to stress, anxiety, and depression. It’s crucial to address mental health as part of comprehensive diabetes care. Support groups and counseling can provide valuable emotional support and coping mechanisms.
- Access to Healthcare: Consistent medical oversight is critical for diabetes management. Access to healthcare services, medications, and monitoring devices can be a significant barrier for some individuals, particularly in low-income or rural areas.
Statistical Insights on the Prevalence of Diabetes Globally
Diabetes is a pervasive health issue with significant global prevalence:
- Global Statistics: According to the International Diabetes Federation, it is estimated that over 537 million adults (20-79 years) were living with diabetes worldwide in 2021, and this number is projected to increase to 643 million by 2030. This staggering increase highlights the urgent need for effective prevention and management strategies.
- Death and Disability: Diabetes is a leading cause of death and disability, contributing to various complications such as cardiovascular disease, kidney failure, and lower limb amputations. It requires comprehensive healthcare strategies to mitigate these outcomes.
- Regional Disparities: The prevalence of diabetes varies greatly between regions, with Southeast Asia, Africa, and the Western Pacific seeing the fastest growth rates. This knowledge stresses the need for targeted interventions tailored to local contexts and healthcare capabilities.
In conclusion, understanding the intricacies of diabetes and its global impact is essential for addressing this chronic illness effectively. Through awareness, education, and comprehensive healthcare strategies, it is possible to improve the quality of life for individuals living with diabetes and reduce the disease’s overall impact on society.

3. The Crucial Role of Self
Managing diabetes is a lifelong journey that requires a proactive approach to living well with the disease. Self-care plays an invaluable role in managing diabetes, providing individuals with the tools and strategies they need to maintain their health and quality of life. Understanding the crucial role of self-care in managing diabetes is essential for those who live with this condition. This guide explores how self-care practices influence diabetes management, highlights effective self-care strategies, and outlines the benefits of self-care in improving the quality of life for diabetes patients.
How Self-Care Practices Influence Diabetes Management
Self-care is pivotal in diabetes management as it empowers individuals to take control of their health. Proactive self-care can lead to better glycemic control, reduce the risk of complications, and improve both physical and mental well-being. Here are some ways self-care practices influence diabetes management:
- Empowerment: By engaging in self-care practices, individuals become active participants in their health management, gaining confidence and autonomy.
- Glycemic Control: Regular monitoring and adjustment of diet and physical activity can help maintain blood glucose levels within the target range.
- Prevention of Complications: Effective self-care reduces the risk of diabetes-related complications such as neuropathy, retinopathy, and cardiovascular disease.
- Overall Health: Self-care encourages a holistic approach, addressing not only blood sugar levels but also other health aspects like nutrition, physical fitness, and mental health.
Examples of Effective Self-Care Strategies for Diabetes
Implementing practical self-care strategies can significantly influence diabetes management. Here are some essential strategies to consider:
- Diet:
A balanced and nutritious diet is foundational in managing diabetes. Focus on: - Incorporating a variety of vegetables, fruits, whole grains, and lean proteins.
- Limiting processed and sugary foods that can spike blood glucose levels.
- Practicing portion control to avoid overeating.
- Monitoring carbohydrate intake to manage blood sugar more effectively.
- Exercise:
Regular physical activity helps improve insulin sensitivity and blood sugar control. Consider: - Engaging in at least 150 minutes of moderate aerobic activity per week, such as walking, swimming, or cycling.
- Incorporating strength training exercises at least two times a week to improve muscle mass and metabolism.
- Finding enjoyable activities to stay consistent with the exercise routine.
- Monitoring Blood Sugar:
Regular blood sugar monitoring is vital. Benefits include: - Understanding how different foods, activities, and stress levels affect blood sugar.
- Making timely adjustments to treatment plans as needed.
- Keeping track of trends and patterns to prevent hyperglycemia or hypoglycemia.
Benefits of Self-Care in Improving Quality of Life for Diabetes Patients
Self-care transcends the physical management of diabetes and profoundly impacts the overall quality of life. Here are some benefits self-care brings to diabetes patients:
- Enhanced Physical Health:
Consistent self-care leads to better physical health outcomes, including a healthy weight, improved cardiovascular health, and increased energy levels. - Improved Emotional Well-being:
Self-care practices such as mindfulness and stress management can reduce anxiety and depression often associated with chronic diseases. - Increased Longevity:
By preventing complications and maintaining good health, self-care contributes to a longer, healthier life. - Greater Satisfaction and Engagement in Life:
Patients often experience improved self-esteem, independence, and satisfaction in daily activities through effective self-care.
In conclusion, self-care is an essential component of diabetes management. Through diet, exercise, and regular monitoring of blood glucose, individuals with diabetes can lead fulfilling and healthy lives. Embracing self-care not only manages the disease effectively but also enhances the overall quality of life for diabetes patients, paving the way for a healthier future.
4. Practical Self
Managing diabetes requires an effective and personalized self-care routine that encompasses diet, physical activity, and medication management. Focusing on these areas, alongside emphasizing mental health and stress management, and leveraging technology can lead to improved outcomes and a higher quality of life for those with diabetes. Here’s a comprehensive guide to practical self-care tips for individuals striving to maintain optimal diabetes management:
Creating a Personalized Self-Care Routine
Diet
A well-balanced diet is critical for managing diabetes effectively. Personalizing your diet plan should involve balancing your macronutrients and monitoring carbohydrate intake to keep blood sugar levels stable. Here’s how you can personalize your dietary plan:
- Understand Carbohydrate Counting: Learn which foods contain carbohydrates and monitor your intake, focusing on high-fiber and whole-grain options which have a lower glycemic index.
- Create a Meal Plan: Tailor meals to your preferences, ensuring a balance of proteins, fats, and carbohydrates. Incorporate a variety of foods to get a range of nutrients.
- Portion Control: Use measuring cups or a food scale to manage portion sizes. This can help in maintaining weight and controlling blood sugar.
Physical Activity
Regular physical activity enhances insulin sensitivity and aids in weight management. Your routine should be tailored to your preferences and physical capabilities:
- Set Realistic Goals: Begin with moderate activities like walking or cycling and gradually increase intensity as you become more fit.
- Incorporate Strength Training: Building muscle can help in better glucose uptake by your body, so include resistance exercises at least twice a week.
- Monitor Blood Sugar Levels: Keep track of how different activities affect your glucose readings to fine-tune your routine.
Medication Management
Managing medication is a critical component of a diabetes self-care plan:
- Regular Medication Reviews: Schedule reviews with healthcare providers to ensure your medication is effectively managing your condition.
- Keep a Medication Log: Record times and dosages of your medications to avoid missing doses or taking them incorrectly.
- Be Prepared for Emergencies: Ensure you have an adequate supply of medications and understand what to do in case of missed doses or emergencies.
Importance of Mental Health and Stress Management
Diabetes can be a physically and mentally taxing condition, making mental health a vital part of your self-care routine:
- Practice Mindfulness and Meditation: Regular mindfulness practices can reduce stress and improve your ability to manage your condition.
- Seek Professional Support: Consider speaking to a therapist for cognitive-behavioral therapy sessions or other professional support to tackle diabetes-related stress.
- Build a Support Network: Reach out to family, friends, or support groups to share experiences and draw encouragement from others managing similar challenges.
Utilizing Technology and Resources for Better Management
Embracing technology can simplify managing diabetes by providing tools for tracking and timely interventions:
- Use Glucose Monitoring Systems: Devices like Continuous Glucose Monitors (CGMs) offer real-time data about your blood sugar, helping you make informed decisions.
- Leverage Mobile Apps: Apps designed for diabetes management can track medications, diet, and physical activity, and provide reminders and educational resources.
- Telemedicine: Access healthcare professionals remotely for consultations and support without the need for frequent in-person visits.
In conclusion, creating a personalized self-care routine and integrating technology and resources significantly enhances diabetes management. By focusing on diet, physical activity, medication management, and mental health, you can better manage your diabetes and improve your overall well-being. Remember, small steps towards change can lead to substantial improvements in managing your condition.