Demystifying Continuous Glucose Monitoring (CGM) Technology For Better Control Of Your Condition
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Understanding Continuous Glucose Monitoring (CGM) Technology
Outline 1: Understanding Continuous Glucose Monitoring (CGM) Technology
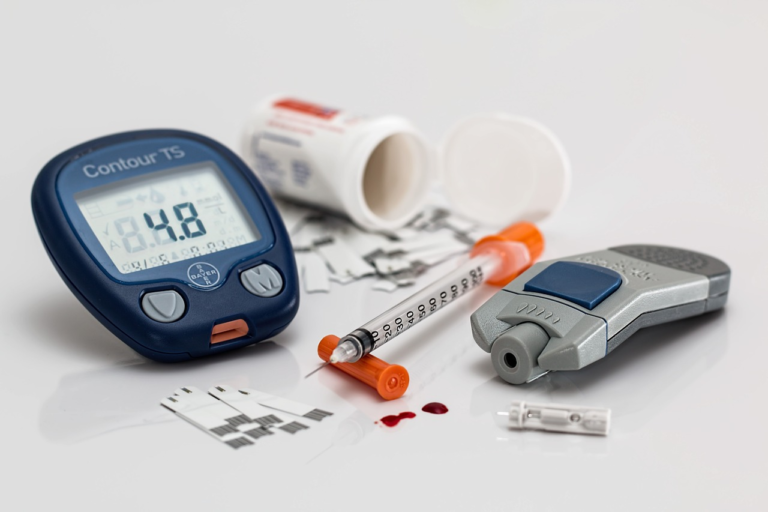
As the prevalence of diabetes continues to rise globally, managing blood glucose levels effectively becomes ever more crucial. Continuous Glucose Monitoring (CGM) technology has emerged as a groundbreaking tool, revolutionizing how individuals with diabetes monitor and manage their condition. In this segment, we delve into the essence of CGM, explore the technology behind popular devices, distinguish it from traditional monitoring methods, and highlight its importance for individuals managing diabetes.
Overview of CGM Devices
Continuous Glucose Monitoring (CGM) involves the use of wearable devices that track glucose levels in real-time throughout the day and night. Unlike traditional methods that only provide snapshots of glucose levels, CGM offers a dynamic picture, enabling better diabetes management. Here are some essential components and features of CGM devices:
- Sensor: A small sensor is inserted just under the skin, typically on the abdomen or upper arm. This sensor measures the glucose levels in interstitial fluid.
- Transmitter: Attaches to the sensor, sending data wirelessly to a receiver or compatible smart device.
- Receiver/Smart Device: Displays real-time glucose data, trends, and patterns, allowing users to gain insights into their glycemic control.
- Alerts and Notifications: Provides customizable alerts for low and high glucose levels, empowering users to take prompt corrective actions.
The advent of CGM technology has introduced a variety of devices from different manufacturers, each offering unique features tailored to the needs of users. Among the popular CGM devices available in the market are the Dexcom G6, Medtronic Guardian Connect, and the FreeStyle Libre systems. These devices vary in sensor duration, calibration requirements, and smartphone compatibility, yet all share the common goal of improving glycemic management.
How CGM Differs from Traditional Glucose Monitoring Methods
Traditional blood glucose monitoring typically involves the use of a glucose meter, lancets, and test strips to obtain a blood sample and measure glucose levels at discrete times. Here’s how CGM stands apart from these conventional methods:
- Frequency and Convenience: CGM provides continuous data, automatically recording glucose levels at 1-5 minute intervals throughout the day. In contrast, traditional monitoring requires conscious effort at specific times and may lead to missed trends between readings.
- Data Insights: The continuous stream of data from CGM offers valuable insights such as glucose trends, patterns, and time-in-range metrics. Traditional methods provide isolated readings without this comprehensive contextual information.
- Reduced Finger Pricks: CGM drastically reduces the need for finger pricks. While occasional calibration may be necessary, the frequency is significantly lower than that of traditional methods.
- Real-time Alerts: CGM devices can be programmed to alert users to impending hypo- or hyperglycemia, enabling proactive management. Traditional meters cannot alert users in real-time.
By offering a holistic view of glucose fluctuations, CGM technology allows users not just to react to glucose excursions but to anticipate and prevent them effectively.
Importance of CGM for Individuals with Diabetes
For individuals with diabetes, CGM technology can be a transformative ally in disease management. Here are several reasons why CGM is critical for diabetic care:
- Better Glycemic Control: The detailed information provided by CGM facilitates informed decision making and tighter control over glucose levels, which can lead to improved HbA1c outcomes.
- Improved Quality of Life: By reducing the burden of frequent finger pricks and offering peace of mind with real-time alerts, CGM enhances the overall quality of life for users.
- Prevention of Complications: CGM assists in maintaining glucose levels within the target range, minimizing risks associated with prolonged hypo- and hyperglycemia, and reducing the likelihood of diabetes-related complications.
- Personalized Education: The data amassed by CGM systems can be shared with healthcare providers, leading to personalized feedback and education, ultimately resulting in more effective diabetes management strategies.
As CGM technology continues to evolve, it holds the promise of further advancements, including longer sensor wear times, integration with insulin pumps, and enhanced data analytics. For individuals living with diabetes, embracing CGM represents not just adopting a new device but embarking on a path toward more informed, empowered, and proactive health management.

2. The Mechanics of CGM: How It Works
The integration of technology into healthcare has revolutionized the management and understanding of various health parameters, particularly for individuals with diabetes. Among these technological advancements, the Continuous Glucose Monitoring (CGM) system stands out as a pivotal tool. It offers a real-time insight into glucose levels, thereby facilitating improved diabetes management. This section delves into the mechanics of CGM systems, elucidating how they work, their components, and how to interpret the data they provide.
The Mechanics of CGM: How It Works
To appreciate the benefits of a CGM system, it’s crucial to understand its mechanics. At its core, a CGM continuously tracks glucose levels, providing valuable data that can help in making informed decisions about diet, exercise, and medication. Here’s a closer look at the key components and functionalities:
Components of a CGM System
A CGM system is comprised of three essential components:
- Sensor: The sensor is a small, flexible piece of equipment inserted under the skin, often in the abdominal area. It’s tasked with measuring glucose levels in the interstitial fluid, which surrounds the cells in your tissues. Despite being minimally invasive, the sensor is highly sensitive and capable of detecting fluctuations in glucose levels.
- Transmitter: This component works hand in hand with the sensor. Once the sensor detects glucose levels, the transmitter sends this information wirelessly to the receiver. Some modern transmitters are integrated into the sensor itself, making the process seamless and efficient.
- Receiver: The final piece of this trio is the receiver, which can be a dedicated device or a smartphone app. It collects data from the transmitter, displaying glucose levels in real-time. This component may also process the data to show trends and graphs, assisting users in understanding their glucose dynamics better.
The Process of Continuous Glucose Measurement
The process of measuring glucose continuously involves several crucial steps:
- Insertion of the Sensor: The sensor is inserted comfortably under the skin, often with the help of a tiny needle. Once in place, it begins to interact with the interstitial fluid to measure glucose concentrations.
- Data Collection: As the sensor measures glucose levels, it converts this information into electrical signals. These signals are then picked up by the transmitter.
- Transmission of Data: The transmitter sends the data wirelessly to the receiver at regular intervals. This communication is facilitated by Bluetooth or other wireless technologies.
- Data Display: The receiver processes the incoming signals and translates them into a user-friendly format. This display allows users to monitor their glucose levels throughout the day seamlessly.
Data Interpretation: Trends, Graphs, and Alerts
A primary benefit of using a CGM system is the ability to interpret vast amounts of data in real-time. Here’s how users can make the most of the insights offered by these systems:
- Understanding Trends: CGMs provide ongoing data, making it easy to observe short-term and long-term glucose trends. By analyzing these patterns, users can identify periods of hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar), and adjust lifestyle or medication accordingly.
- Utilizing Graphs: Many CGMs translate data into easy-to-read graphs. These visual representations help users and healthcare providers pinpoint trends and make informed decisions regarding treatment plans.
- Setting Alerts: Modern CGM systems allow users to set customizable alerts. These notifications warn users when their glucose levels exceed or fall below predetermined thresholds, urging prompt corrective actions.
By marrying advanced technology with intuitive user interfaces, CGM systems offer a comprehensive approach to diabetes management. For individuals with diabetes, these systems are not just tools but companions that provide the confidence and data they need to navigate their day-to-day lives with greater ease and fewer disruptions. Whether through detailed trends, precise graphs, or timely alerts, the capabilities of CGMs are continually expanding, pushing the boundaries of what’s possible in health monitoring.

3. Benefits of Using CGM Technology for Managing Diabetes
Continuous Glucose Monitoring (CGM) technology has revolutionized diabetes management, offering individuals real-time insights into their glucose levels. This cutting-edge approach not only enhances glycemic control but also plays a pivotal role in reducing diabetes-related complications. Moreover, CGM provides an in-depth understanding of how diet, exercise, and medication impact glucose levels, empowering patients to make informed decisions.
Benefits of Using CGM Technology for Managing Diabetes
Real-Time Glucose Level Monitoring and Its Impact on Lifestyle
The integration of CGM technology into diabetes management offers unprecedented benefits. By providing continuous, real-time data, CGM devices allow individuals to track glucose level trends and patterns. This leads to several lifestyle improvements:
- Immediate Feedback: Instead of waiting for periodic finger-prick tests, users receive instant feedback on how lifestyle choices affect their glucose levels.
- Proactive Management: With real-time insights, individuals can take immediate action, such as adjusting their insulin or opting for a brisk walk to reduce high glucose levels.
- Improved Awareness: Understanding how meals, stress, and exercise affect glucose levels helps patients tailor their daily activities to maintain optimal health.
Overall, real-time glucose monitoring significantly impacts lifestyle choices, allowing diabetics to maintain more stable glucose levels and thus leading to improved well-being.
Improving Glycemic Control and Reducing Diabetes-Related Complications
Consistent glycemic control is crucial in minimizing the risk of complications associated with diabetes, such as neuropathy, retinopathy, and cardiovascular diseases. CGM technology facilitates this control through:
- Better Identification of Patterns: By providing comprehensive glucose profiles, CGM helps in identifying hyperglycemia and hypoglycemia patterns, enabling tailored treatment strategies.
- Reduced HbA1c Levels: Studies show that CGM users often experience significant reductions in HbA1c levels, a key indicator of long-term glucose control.
- Prevention of Severe Hypoglycemia: Alerts for low glucose levels ensure timely interventions, preventing severe hypoglycemic episodes that can be life-threatening.
As a result, CGM effectively supports better glycemic control, thereby decreasing the likelihood of diabetes-related complications.
Enhanced Decision-Making in Diet, Exercise, and Medication Management
CGM is not just a tool for monitoring glucose levels; it is an invaluable resource for decision-making concerning diet, exercise, and medication. Here’s how:
-
Diet Management:
- Users can observe firsthand how different foods impact their glucose levels and adjust their dietary choices accordingly.
- Real-time data helps in formulating personalized diet plans that promote stable blood glucose levels.
-
Exercise Management:
- CGM provides insights into how different forms of exercise affect glucose, aiding in the planning of workout routines for optimal glucose control.
- Individuals can detect immediate glucose changes post-exercise, helping to prevent exercise-induced hypoglycemia.
-
Medication Management:
- With CGM, patients and healthcare providers can refine medication administration timing and dosage based on real-time glucose data.
- This helps in achieving a more precise balance between insulin and blood glucose levels.
The result is a more informed approach to diabetes management, leading to enhanced quality of life and better health outcomes.
In conclusion, the benefits of CGM technology in managing diabetes are undeniable. From real-time glucose monitoring to improving glycemic control and enhancing decision-making processes regarding diet, exercise, and medication, CGM has a profound impact on the lifestyle and health of individuals managing diabetes.
4. Overcoming Challenges and Maximizing the Use of CGM
“`html
Overcoming Challenges and Maximizing the Use of CGM
Continuous Glucose Monitoring (CGM) technology has revolutionized diabetes management by providing real-time insights into glucose levels. However, despite its benefits, several misconceptions and barriers can hinder its adoption. This segment addresses these challenges and provides actionable tips for integrating CGM into daily routines, alongside understanding the insurance coverage and financial aspects involved.
Addressing Common Misconceptions and Barriers to Adoption
Many potential users of CGM hesitate due to various misconceptions. Addressing these can help maximize the benefits that CGM technology offers:
-
Misconception 1: CGM is too complicated.
Some believe CGM devices are overly complex. However, most modern systems are user-friendly, with dashboards that simplify data interpretation. Healthcare professionals offer guidance to make the transition smoother.
-
Misconception 2: CGM is uncomfortable and invasive.
While it’s true that CGM involves wearing a sensor that stays on the skin, most users find it to be minimally invasive and quickly get accustomed to wearing it.
-
Barrier: Cost and insurance issues.
Costs can be a significant barrier; thus, understanding insurance policies is crucial. Many insurances are increasingly covering CGM as its importance in diabetes care is recognized.
-
Barrier: Data Overload.
Initially, the sheer amount of data from CGM can be overwhelming. Users should gradually familiarize themselves with interpreting this data to aid decision-making.
Tips for Integrating CGM into Daily Routines
Once the decision to use CGM has been made, integrating it into daily life effectively is essential for maximizing its benefits:
-
Start Slowly: Introduce CGM into your routine gradually. Begin by using the alerts and trends to learn how different activities affect your glucose levels.
-
Customize Your Settings: Set personalized alerts that notify you of high or low glucose levels. Tailor these alerts to your lifestyle and activity level.
-
Consistent Monitoring: Regularly review your data to identify patterns and trends. This information will help you adjust your diet, exercise, and medication more effectively.
-
Regular Consultations: Follow up with healthcare professionals to discuss your CGT data. They can provide medical advice tailored to your specific needs and enhance your glucose management strategies.
-
Share Data with Family Members: Many CGM solutions allow data sharing, which can be beneficial if family members need to support your glucose management.
Understanding Insurance Coverage and Financial Aspects
Navigating the financial aspects of CGM is essential for many users. Here’s how to effectively manage these concerns:
-
Insurance Coverage: Many insurers view CGM as an essential tool for diabetes management and may cover its costs. It’s advisable to:
- Contact your insurance provider directly to get a detailed explanation of your policy regarding CGM.
- Ask about the need for prior authorization or physician referrals, as these can affect coverage.
- Inquire about the specifics, such as whether both sensors and readers are covered.
-
Leverage Financial Assistance Programs: Manufacturers and nonprofit organizations often offer financial aid programs to assist with unmanageable costs. Research and apply for these programs if necessary.
-
Consider Device Warranties and Replacement Policies: Understanding the warranties on CGM devices can save costs in the long run, should any part of the device need replacement.
-
Discuss with an Endocrinologist: Medical professionals can advocate on your behalf for insurance coverage, offering necessary documentation stating the medical need for CGM.
Integrating CGM into your diabetes management strategy offers significant benefits but requires overcoming common misconceptions, incorporating the device into your daily routine thoughtfully, and understanding the financial landscape. Embrace these steps to fully harness the potential of CGM technology, thereby enhancing your quality of life.
“`