Finding Balance: Managing Your Mental Health as a Person With diabetes
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Mental Health Challenges for People with Diabetes
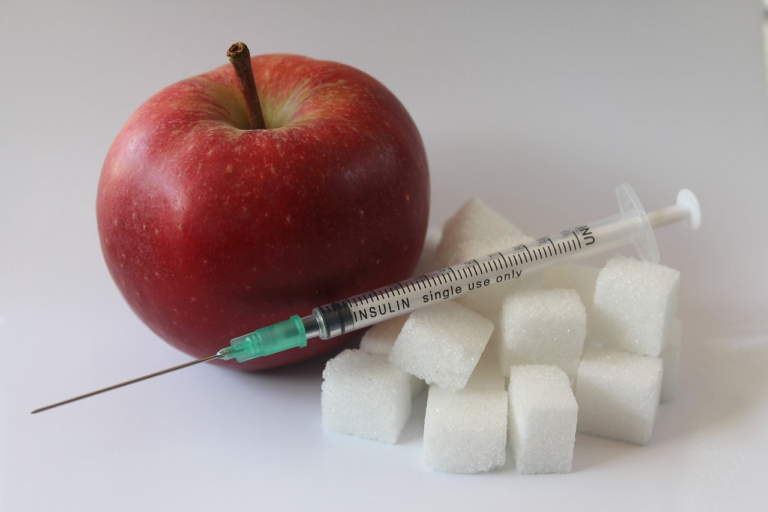
Diabetes, a chronic illness characterized by the body’s inability to properly process blood glucose, is often understood in terms of its physical implications. However, there’s a crucial dimension to living with diabetes that requires equal attention: mental health. Individuals with diabetes frequently face mental health challenges such as stress, anxiety, and depression. This segment will explore the connection between diabetes and mental health issues, discuss the importance of mental well-being in diabetes management, and introduce the concept of finding balance between physical and mental health.
Overview of the Connection between Diabetes and Mental Health Issues
The relationship between diabetes and mental health is a complex, multifaceted one. Managing a chronic condition like diabetes is inherently stressful, necessitating constant vigilance about blood sugar levels, medication, diet, and exercise. This constant attention can lead to stress, anxiety, and ultimately, mental health struggles.
- Stress: The demands of diabetes management can lead to a persistent state of stress. Tracking blood sugars, counting carbohydrates, and planning meals and activities around insulin requirements is no small feat, often leaving individuals feeling overwhelmed.
- Anxiety: Anxiety can arise from the fear of hypoglycemic episodes, complications, or the impacts of the disease on daily life. This anxiety may result in avoidance of activities or situations, significantly impacting the quality of life.
- Depression: The burden of living with diabetes increases the risk of depression. Studies indicate that people with diabetes are more likely to experience depression than those without the condition. Depression can further complicate diabetes management, making it harder to stick to treatment plans and maintain healthy habits.
Addressing these mental health challenges is critical because they directly impact diabetes management outcomes. Poor mental health can result in suboptimal self-care, leading to a vicious cycle where blood sugar control deteriorates, further worsening mental health.
Importance of Mental Well-Being in Diabetes Management
Mental health is not just a side issue in diabetes care—it is a core component. Effective diabetes management requires a holistic approach that considers mental well-being as pivotal to achieving optimal health outcomes. Here’s why mental well-being is so important:
- Improved Blood Glucose Control: When individuals have good mental health, they are more likely to adhere to their diabetes management plans, including medication, diet, and exercise. This adherence leads to improved blood glucose levels and reduces the risk of complications.
- Enhanced Quality of Life: Good mental health improves overall quality of life, helping individuals feel more in control of their diabetes and less overwhelmed by daily management tasks. This empowerment leads to greater engagement in social activities and personal interests.
- Reduced Risk of Complications: By managing both mental health and diabetes, individuals can reduce their risk of developing long-term diabetes complications such as cardiovascular disease, neuropathy, and retinopathy.
The integration of mental health care into diabetes treatment plans is essential. This can involve regular mental health screenings, access to counseling and support groups, and the inclusion of stress-reduction techniques such as mindfulness and physical activity in treatment plans.
Finding Balance: Managing Both Physical and Mental Health
The concept of balance becomes particularly important when managing both physical and mental health in diabetes. Finding this balance means giving equal attention to both aspects of health, recognizing that one cannot thrive without the other. Here’s a brief introduction to practices that can aid in achieving this equilibrium:
- Integrated Care Plans: Engage with healthcare providers who recognize the importance of mental health in diabetes care. An integrated care plan that addresses both physical and mental health needs can provide comprehensive support.
- Self-care Techniques: Incorporate relaxation techniques, such as mindfulness and meditation, into daily routines. These practices can help reduce stress and anxiety, promoting a sense of calm that positively influences diabetes management.
- Education and Support: Educate yourself about the mental health challenges associated with diabetes and seek support from peers or support groups. Sharing experiences with others facing similar challenges can provide comfort and practical advice.
- Routine Physical Activity: Exercise is not only vital for physical health but also for cognitive function and emotional well-being. Regular physical activity can reduce symptoms of anxiety and depression while improving metabolic control.
In conclusion, addressing mental health challenges in diabetes is as important as managing the physical symptoms of the disease. By understanding the connection between diabetes and mental health issues, prioritizing mental well-being in diabetes management, and actively pursuing a balanced approach, individuals can lead healthier, more fulfilling lives. As research continues to evolve, it is imperative for healthcare providers and patients alike to remain informed and proactive in integrating mental health care into diabetes management plans.

2. Understanding the Psychological Impact of Diabetes
Diabetes, a chronic illness that affects millions worldwide, poses several psychological challenges alongside its well-known physical complications. Understanding these psychological impacts is crucial as they profoundly influence a person’s ability to manage their condition effectively.
Common Psychological Challenges Faced by Individuals with Diabetes
People living with diabetes often encounter a unique set of psychological challenges. These challenges can complicate disease management and affect overall quality of life. Below, we explore some of the primary psychological issues that individuals with diabetes may face:
- Anxiety and Fear: The constant need to monitor blood sugar levels and the fear of complications can lead to persistent anxiety.
- Depression: The burden of dealing with a chronic illness can lead to feelings of hopelessness and depression.
- Diabetes Distress: A specific emotional response to living with diabetes that includes stress, guilt, or denial about the condition.
- Burnout: The continuous self-care required for diabetes can lead to emotional exhaustion and burnout.
The Burden of Constant Diabetes Management and Its Effects on Mental Health
The relentless nature of diabetes management often takes a toll on an individual’s mental health. The everyday responsibilities include monitoring blood glucose levels, adhering to a strict medication regimen, managing diet, and regular physical activity. These demands can lead to:
- Chronic Stress: Ongoing stress related to managing insulin schedules, dietary restrictions, and regular healthcare appointments.
- Social Isolation: Individuals might feel isolated due to dietary restrictions or fatigue, affecting social interactions and support networks.
- Low Self-Esteem: The constant vigilance required can sometimes lead to feelings of inadequacy or failure if targets are not met.
The burden of these daily tasks can exacerbate common psychological challenges, making it harder for individuals to maintain mental well-being.
Prevalence of Mental Health Conditions in Diabetes Patients
The intersection of diabetes and mental health has been highlighted by various studies, which underscore the prevalence of mental health issues within this community.
- Anxiety Disorders: According to a study published in the journal Diabetes Care, anxiety disorders occur in approximately 20% of individuals with diabetes.
- Depression: The American Diabetes Association notes that people with diabetes are 2 to 3 times more likely to have depression than those without diabetes.
- Diabetes Distress: The prevalence of diabetes distress is estimated to affect 18% to 45% of diabetes patients, as noted in a study in the Journal of Diabetes and Its Complications.
- Burnout: Emotional exhaustion linked to burnout affects around 44% of adults with type 1 diabetes, as detailed by the International Diabetes Federation.
These statistics highlight the significant mental health challenges that accompany diabetes, underscoring the need for integrated care approaches that address both physical and psychological health aspects.
By acknowledging and addressing the psychological impact of diabetes, healthcare providers can better support their patients in managing this complex condition. Collaborative care models that combine endocrinological and psychological expertise can play a critical role in improving outcomes for those living with diabetes.

3. Strategies for Managing Mental Health Alongside Diabetes
Living with diabetes can be a balancing act, requiring not just physical management but also a keen focus on mental health. Stress due to diabetes care and lifestyle adjustments can contribute to mental health challenges, making stress management a critical component of a holistic diabetes care plan. This guide explores effective strategies for managing mental health alongside diabetes, offering practical tips for stress reduction, mindfulness, relaxation, and the importance of professional support.
Stress Management Techniques Tailored for Diabetes Patients
Stress can significantly impact blood glucose levels, as the hormones released during stress can increase insulin resistance. Therefore, managing stress is not only a matter of mental well-being but also a critical factor in diabetes management.
- Physical Activity: Engaging in regular physical activity is a powerful way to relieve stress. Exercise helps lower blood sugar levels and improves insulin sensitivity. Incorporate gentle exercises like walking, swimming, or yoga into your daily routine to keep stress at bay.
- Deep Breathing Exercises: Deep breathing is a simple yet effective stress reduction technique. Practice deep breathing exercises by inhaling slowly through the nose, holding the breath for a few moments, and then exhaling completely. This can be done in a few minutes whenever you feel stressed.
- Time Management: Diabetes care can be time-consuming, and poor time management can lead to stress. Create a schedule for your daily tasks and diabetes management activities to ensure you have enough time to take care of yourself without feeling rushed.
- Healthy Lifestyle Choices: Prioritize a balanced diet and adequate sleep along with regular physical activity. Avoid excessive caffeine and sugar, and aim for at least 7-8 hours of sleep per night. These choices help in creating a stable environment for mental wellness.
Tips for Incorporating Mindfulness and Relaxation Practices into Daily Routines
Mindfulness and relaxation are effective tools for reducing stress and enhancing well-being. Integrating these practices into daily routines can help diabetic patients maintain a clearer focus and better resilience.
- Mindful Eating: Paying attention to the taste, aroma, and texture of the food not only enhances enjoyment but also helps in recognizing hunger cues and portion control, which are vital aspects of diabetes management.
- Yoga and Meditation: Both practices are excellent for reducing stress and increasing concentration. Allocate 10-15 minutes every day for meditation or a yoga routine focused on breathing and relaxation. This can be a relaxed part of your morning routine or a way to unwind in the evening.
- Progressive Muscle Relaxation: This technique involves slowly tensing and then relaxing each muscle group in the body. It helps identify areas of tension and release stress, bringing the body to a more relaxed state, which can aid in better blood sugar control.
- Gratitude Journaling: Keeping a journal to regularly write down things you’re grateful for can shift the focus away from stressors to positive aspects of life. This practice can enhance mood and foster a more positive outlook.
Importance of Seeking Support from Healthcare Professionals and Mental Health Resources
While self-management strategies are crucial, the support of healthcare professionals and mental health resources should not be underestimated. Engaging with healthcare providers can offer a structured approach to managing diabetes and associated mental health issues.
- Regular Consultations: Keep up with regular check-ins with your doctor or diabetes specialist. These appointments are vital not only for monitoring physical health but also for discussing any emotional or mental health concerns.
- Mental Health Professionals: Don’t hesitate to seek guidance from psychologists or counselors who specialize in the mental health impact of chronic diseases. They can provide coping strategies, therapeutic support, and interventions tailored to diabetes patients.
- Support Groups: Joining a diabetes support group can provide a sense of community and shared understanding. These groups are valuable for exchanging tips, emotional support, and learning from others’ experiences.
- Educational Resources: Make use of the educational materials provided by healthcare organizations. They often have comprehensive guides and tips for managing stress and mental health, specifically crafted for individuals with diabetes.
In conclusion, managing mental health alongside diabetes involves a multifaceted approach that includes stress reduction strategies, mindfulness, and relaxation practices, as well as professional support. By incorporating these elements into everyday life, diabetes patients can achieve better mental and physical health outcomes, leading to a more balanced and fulfilling life.
4. Creating a Balanced Routine to Support Mental Well
Creating a Balanced Routine to Support Mental Well-being
In today’s fast-paced world, maintaining mental well-being is crucial for a happy and fulfilling life. At the core of achieving mental health is a structured lifestyle that encompasses a balanced diet, regular exercise, and adequate sleep. These foundational elements contribute to both physical and mental health, making it imperative to integrate them into your daily routine.
The Importance of a Structured Lifestyle Encompassing Diet, Exercise, and Sleep
A structured lifestyle provides stability and predictability, which can significantly reduce stress and anxiety. Here’s how diet, exercise, and sleep play pivotal roles in your overall health:
- Diet: Eating a balanced diet rich in vitamins, minerals, and antioxidants can reduce inflammation and oxidative stress, offering protection against mental health disorders. Foods rich in omega-3 fatty acids, such as fish, nuts, and seeds, have been shown to enhance brain function and mood stability.
- Exercise: Regular physical activity promotes the release of endorphins, the body’s natural mood lifters. It helps reduce symptoms of depression and anxiety and improves sleep quality, leading to better emotional well-being.
- Sleep: Quality sleep is fundamental to mental health. It is essential to have a regular sleep schedule to synchronize the body’s circadian rhythms, supporting cognitive function and emotional resilience.
Setting Realistic Goals and Maintaining a Positive Outlook
Establishing a balanced lifestyle begins with setting realistic goals. Unrealistic goals can lead to frustration and burnout, whereas attainable goals enhance motivation and encourage perseverance. Here are some suggestions:
- Define Clear Objectives: Break down your goals into smaller, manageable tasks. For example, if your goal is to incorporate exercise into your daily routine, start with a 10-minute walk daily before gradually increasing the duration.
- Track Your Progress: Keeping a journal or using apps to log your achievements can provide motivation by showcasing your progress over time.
- Celebrate Small Wins: Acknowledge and celebrate your achievements, no matter how minor. This celebration reinforces positive behavior and boosts self-confidence.
- Stay Positive: Cultivate a positive mindset by practicing gratitude and focusing on positive aspects of your life. Meditation and mindfulness can further enhance resilience and reduce stress.
Benefits of Community Support Groups and Diabetes-Centered Wellness Programs
Engaging with community support groups and participating in wellness programs can offer tremendous benefits to individuals seeking mental well-being, especially for those managing conditions like diabetes.
- Shared Experiences: Support groups provide a platform for individuals to share personal experiences and challenges. This sense of camaraderie can diminish feelings of isolation and reinforce that you are not alone in your journey.
- Expert Guidance: Diabetes-centered wellness programs typically involve healthcare professionals who offer valuable education and tips for managing diet, exercise, and lifestyle changes effectively.
- Accountability: Being part of a group fosters accountability. Regular meetings or check-ins can motivate you to stay on course with your health and wellness goals.
- Enhanced Motivation: Interacting with individuals on a similar journey can inspire you to keep pushing forward, even on challenging days. Seeing others’ progress can kindle your motivation to achieve your personal wellness objectives.
In conclusion, creating a balanced routine encompassing diet, exercise, and sleep is vital for supporting mental well-being. By setting realistic goals, maintaining a positive outlook, and tapping into the power of community support groups and wellness programs, individuals can enhance their mental health and enjoy a more fulfilling life. Embrace these strategies today and take meaningful steps towards achieving optimal mental well-being.