From Diagnosis to Remission? Understanding the Potential Cure For Some Types Of diabetes
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Diabetes: Types and Challenges
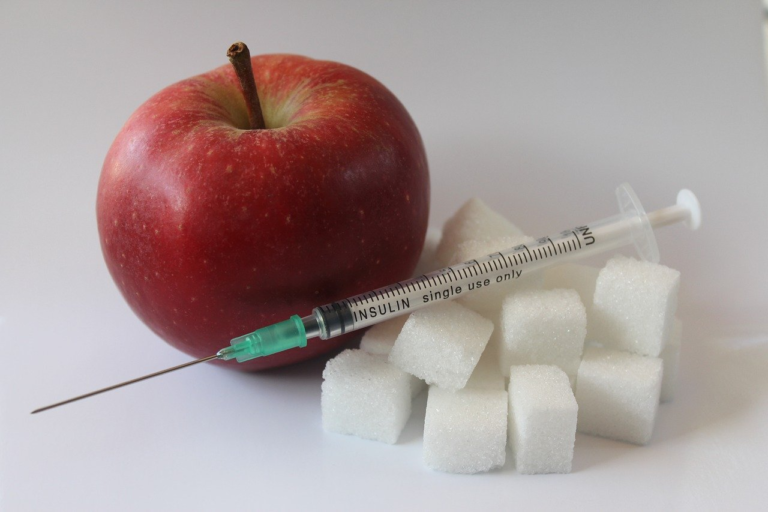
Diabetes is a chronic disease that affects millions of people worldwide, making it one of the largest global health emergencies of the 21st century. It occurs when the body is unable to effectively use or produce the hormone insulin, leading to elevated levels of glucose in the blood. Recognizing the implications and the scale of this disease is imperative for managing it effectively.
Understanding diabetes begins with grasping its types and the unique challenges each presents. Let’s dive into an overview of diabetes, explore the distinction between type 1 and type 2 diabetes, and examine the current challenges in managing this disease effectively.
Overview of Diabetes and Its Prevalence Worldwide
Diabetes is a major public health concern, impacting populations across the globe. According to recent statistics:
- Approximately 463 million adults were living with diabetes in 2019, and this number is expected to rise to 700 million by 2045.
- In countries such as China, India, and the United States, diabetes prevalence is particularly high.
- Diabetes directly caused 1.5 million deaths in 2019.
Given these staggering figures, it’s evident that diabetes is not just a health issue but a socio-economic challenge affecting both individuals and healthcare systems worldwide.
The Distinction Between Type 1 and Type 2 Diabetes
Understanding the difference between type 1 and type 2 diabetes is crucial for effective management and intervention:
- Type 1 Diabetes
- This type is often diagnosed in children and young adults, and it is characterized by the body’s inability to produce insulin.
- The cause is not entirely understood but is believed to involve a combination of genetic predisposition and environmental factors.
- Individuals with type 1 diabetes must take insulin injections for life and closely monitor their blood glucose levels.
- Type 2 Diabetes
- This is the most common type of diabetes, accounting for about 90% of all cases globally.
- It is primarily associated with obesity, sedentary lifestyle, and poor dietary habits.
- Unlike type 1, type 2 diabetes results from the body becoming resistant to insulin, thus demanding lifestyle changes along with medical interventions for management.
Each type of diabetes requires a different management approach, impacting diet, exercise, and medication strategies.
Current Challenges in Managing Diabetes Effectively
Despite advancements in medical science, managing diabetes presents numerous challenges:
- Access to Healthcare: Not all individuals have equal access to healthcare facilities and educational resources essential for diabetes management.
- Cost of Treatment: Diabetes is associated with substantial financial burdens due to the ongoing need for medication, monitoring equipment, and healthcare services.
- Lifestyle Changes: Embracing necessary lifestyle alterations, including diet and physical activity, proves difficult for many.
- Technological Barriers: While technology offers advanced glucose monitoring and insulin delivery systems, they are not universally available due to cost and lack of accessibility.
- Complications Management: Diabetes increases the risk of various complications, such as cardiovascular disease, neuropathy, and eye diseases, all requiring vigilant monitoring and intervention.
To combat these challenges effectively, a comprehensive approach involving policy change, education, and sustained research is essential.
In summary, diabetes is a multifaceted disease with far-reaching impacts. Understanding its types and the unique challenges associated with each is crucial for implementing effective preventive and management strategies. As the prevalence of diabetes continues to rise globally, addressing these challenges with innovation and inclusivity remains a pivotal task for medical professionals, policymakers, and educators alike.

2. The Journey from Diagnosis to Treatment
Diabetes, a chronic metabolic condition characterized by elevated blood sugar levels, demands a comprehensive understanding of its journey from diagnosis to treatment. This segment delves into the essential steps involved in diagnosing diabetes, explores the conventional treatment methods and their limitations, and underscores the importance of early diagnosis in effective diabetes management.
The Journey from Diagnosis to Treatment
Steps Involved in Diagnosing Diabetes
Diagnosing diabetes is a critical first step in managing the condition. Here are the key steps involved in the diagnosis:
- Symptom Evaluation: The process begins with the evaluation of symptoms. Common symptoms of diabetes include increased thirst, frequent urination, extreme fatigue, blurred vision, and slow-healing sores.
- Medical History: A detailed medical history is gathered to assess the risk factors, such as family history, obesity, or sedentary lifestyle, contributing to the development of diabetes.
- Physical Examination: A thorough physical examination helps in identifying signs that align with diabetes, like acanthosis nigricans, a skin condition indicating insulin resistance.
- Blood Glucose Tests: Several blood tests are utilized to confirm the diagnosis:
- Fasting Blood Sugar (FBS) Test: Measures blood sugar levels after an overnight fast. A fasting glucose level of 126 mg/dL or higher suggests diabetes.
- Oral Glucose Tolerance Test (OGTT): Blood sugar levels are checked before and two hours after consuming a glucose-rich drink. A level of 200 mg/dL or higher after the test indicates diabetes.
- Hemoglobin A1C Test: Reflects the average blood sugar level over the past two to three months. An A1C level of 6.5% or higher confirms diabetes.
- Additional Tests: In some cases, additional tests may be conducted, such as urine tests for ketones or C-peptide tests to assess insulin production.
Conventional Treatment Methods and Their Limitations
Once diagnosed, diabetes management primarily involves conventional treatment methods. While these have been effective to some extent, they also have limitations:
- Medications:
- Insulin Therapy: Vital for type 1 diabetes and some cases of type 2 diabetes, insulin helps regulate blood sugar. However, it requires meticulous monitoring and can lead to hypoglycemia if not balanced correctly.
- Oral Hypoglycemics: Drugs like metformin and sulfonylureas assist in controlling blood sugar levels. But, they may cause side effects such as gastrointestinal issues or weight gain.
- Lifestyle Modifications: Healthy eating, regular physical activity, and weight management are fundamental aspects of lifestyle changes for diabetes management. Adhering to these can be challenging for many individuals.
- Blood Sugar Monitoring: Regular monitoring of blood glucose levels is crucial for managing diabetes. However, this demands diligence and can lead to stress or anxiety in some patients.
- Limitations: Conventional treatments often do not address the underlying causes of insulin resistance or beta-cell dysfunction. Additionally, they may not fully prevent diabetes-related complications over time.
The Importance of Early Diagnosis in Diabetes Management
Early diagnosis of diabetes plays a pivotal role in the effective management of the condition. Here’s why it is crucial:
- Prevention of Complications: Early detection allows for the immediate initiation of treatment plans, reducing the risk of long-term complications such as cardiovascular disease, neuropathy, and retinopathy.
- Improved Quality of Life: Timely diagnosis and intervention can significantly enhance an individual’s quality of life by controlling symptoms and preventing disease progression.
- Cost-Effectiveness: Managing diabetes in its early stages is more cost-effective than treating advanced complications, leading to reduced healthcare expenses over time.
- Behavior Modification: Early diagnosis often serves as a wake-up call, motivating individuals to adopt healthier lifestyle choices that can halt or slow down disease progression.
- Tailored Treatment Plans: Recognizing diabetes early allows healthcare providers to design personalized treatment strategies that address the unique needs of each patient, potentially enhancing treatment outcomes.
In conclusion, while conventional treatments for diabetes have provided significant benefits, their limitations underscore the critical importance of early diagnosis. By catching the disease in its initial stages, patients have a greater opportunity to manage their condition effectively, minimizing complications and improving overall health outcomes.

3. Advances in Diabetes Research: Hope for a Cure
Diabetes research has made significant strides in recent years, offering renewed hope for a cure and improving the quality of life for millions affected by this chronic condition. The advances range from breakthrough treatments to innovative therapies that aim to achieve remission. This article delves into recent developments and showcases successful case studies to highlight the progress being made in the fight against diabetes.
Recent Breakthroughs in Diabetes Treatment and Research
Scientific research continues to push the boundaries of what is achievable in diabetes treatment. Recent breakthroughs have focused on improving current therapies and developing novel interventions that target the disease’s root causes.
- Stem Cell Therapy: Researchers have made headway in stem cell therapy, a groundbreaking approach that involves reprogramming stem cells to produce insulin. This technique has shown promise in early-stage trials, offering the potential for long-term remission of Type 1 diabetes.
- Artificial Pancreas: The introduction of advanced insulin pumps and continuous glucose monitoring systems has paved the way for the development of an artificial pancreas. These closed-loop systems mimic the function of a healthy pancreas, automating insulin delivery and significantly improving blood glucose control.
- Gene Editing: CRISPR gene-editing technology has opened the door to correcting genetic mutations associated with diabetes. This approach could potentially prevent or reverse the progression of the disease.
Innovative Therapies Aimed at Achieving Remission
Innovative therapies are not only managing diabetes symptoms but also targeting remission. Remission is defined as the maintenance of normal blood glucose levels without the need for medication. Here are some groundbreaking therapies paving the way towards this goal:
- Immunotherapy: By modulating the body’s immune response, immunotherapy aims to preserve and restore insulin production in people with Type 1 diabetes. Clinical trials have shown promising results, with some patients achieving partial remission.
- Metabolic Surgery: Initially designed for weight loss, metabolic surgery has demonstrated remarkable outcomes in achieving remission in Type 2 diabetes patients, often improving glucose levels long-term.
- Gut Microbiota Modulation: Modifying the gut microbiome through probiotics and dietary interventions is being explored as a tool for improving insulin sensitivity and achieving diabetes remission.
Case Studies Highlighting Successful Remission
Real-world examples provide compelling evidence of the progress made in managing diabetes. Here, we present case studies that highlight successful remissions achieved through innovative therapies.
- Case Study 1: John’s Recovery Through Stem Cell Therapy
- Background: John, a 45-year-old with Type 1 diabetes, participated in a clinical trial involving stem cell therapy.
- Treatment: He underwent a series of stem cell infusions aiming to regenerate insulin-producing cells.
- Outcome: Over 18 months, John experienced a significant reduction in insulin requirements and maintained stable glucose levels.
- Case Study 2: Emily’s Journey with Metabolic Surgery
- Background: Emily, aged 38, was diagnosed with Type 2 diabetes at an early age and struggled with obesity.
- Treatment: She underwent gastric bypass surgery, which significantly impacted her glucose metabolism.
- Outcome: Post-surgery, Emily’s blood sugar levels normalized, and she achieved remission without additional medication.
- Case Study 3: David’s Success with Immunotherapy
- Background: David was diagnosed with Type 1 diabetes as a teenager.
- Treatment: He participated in an immunotherapy clinical trial targeting autoimmune responses.
- Outcome: The treatment halted further destruction of insulin-producing cells, and David achieved partial remission, significantly reducing his insulin usage.
The landscape of diabetes research is rapidly evolving, backed by the collective efforts of scientists, clinicians, and patients. These advances represent a beacon of hope, suggesting that a cure for diabetes might one day become a reality. As research continues to unravel the complexities of this disease, the prospect of achieving widespread remission grows ever more promising.
4. Understanding Remission in Diabetes
Understanding remission in diabetes is crucial for anyone looking to manage or overcome this chronic condition. Unlike a cure, remission implies a significant reduction or disappearance of symptoms. In this segment, we’ll explore what remission means in diabetes, the factors contributing to successful remission, and the medical distinctions between remission and a cure.
Definition and Significance of Diabetes Remission
Diabetes remission represents a state where someone with diabetes achieves blood glucose levels below the diabetic range without the use of any diabetes medication. This state must be maintained for at least a year for it to be classified as remission. While this doesn’t mean that diabetes is cured, it signals a profound improvement in overall health and metabolic function.
The significance of diabetes remission can be highlighted in various ways:
- Improved Health Outcomes: Achieving remission can result in better glycemic control, reducing the risk of diabetic complications such as neuropathy, retinopathy, and cardiovascular diseases.
- Reduced Medication Dependence: Patients in remission might not require diabetes medication, significantly improving their quality of life.
- Cost Savings: Less reliance on medication and fewer diabetes-related complications can result in lower healthcare costs for both individuals and healthcare systems.
- Psychological Benefits: Entering remission can improve mental health, increasing motivation and overall life satisfaction.
Factors Contributing to Successful Remission
Achieving diabetes remission is not guaranteed, but various factors can increase the likelihood of entering and maintaining this state. Here are some key components:
- Weight Management: Losing significant weight has been shown to help put type 2 diabetes into remission. Maintaining a healthy weight is crucial for those attempting remission.
- Diet: A balanced diet, particularly one low in refined sugars and carbohydrates, can support blood sugar control, potentially aiding remission. This might include Mediterranean, ketogenic, or plant-based diets.
- Physical Activity: Regular exercise helps improve insulin sensitivity, aiding in blood sugar management and possibly leading to remission.
- Bariatric Surgery: For some individuals, particularly those with obesity, bariatric surgery can lead to remission of type 2 diabetes.
- Early Intervention: Early diagnosis and treatment of type 2 diabetes increase the chances of successful remission through lifestyle changes and medical interventions.
Distinctions Between Remission and Cure in a Medical Context
Understanding the difference between remission and a cure is vital in the context of diabetes and other chronic conditions. Here’s how these terms differ:
- Remission: In diabetes, remission signifies that blood glucose levels are maintained within a normal range without medication. However, the underlying vulnerability to diabetes doesn’t disappear, indicating a propensity for relapse if lifestyle modifications are not maintained.
- Cure: A cure means that the disease is completely eradicated, and there’s no chance of relapse. In diabetes, particularly type 1, there is currently no cure as the underlying autoimmune processes are not reversible.
Doctors emphasize that while achieving remission is a significant step, it’s crucial for individuals to continue healthy lifestyle practices to sustain remission and prevent a relapse.
Recognizing these factors and distinctions empowers patients and healthcare providers to approach diabetes management more effectively, aiming for remission where possible while continuing to search for more permanent solutions or cures in the field.