How Support Groups Can Improve Quality Of Life For People Living With gestational diabetics
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Gestational Diabetes and Its Impact on Quality of Life
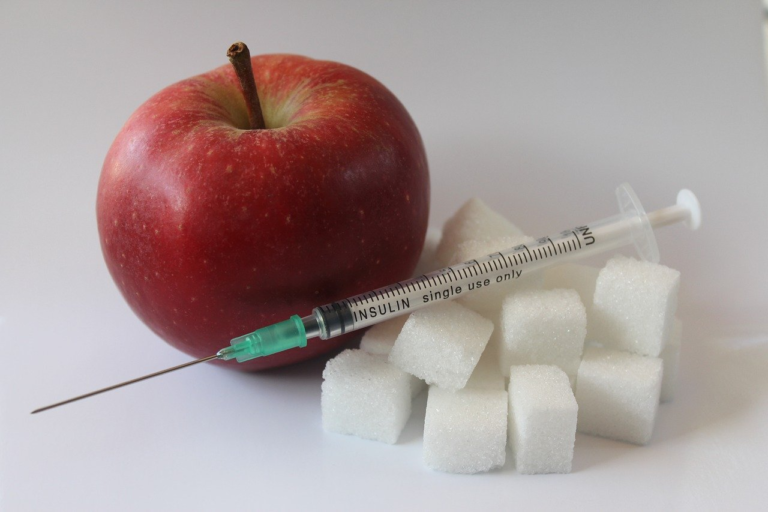
Gestational diabetes mellitus (GDM) is a significant health concern that emerges during pregnancy, characterized by glucose intolerance that is first recognized or diagnosed during pregnancy. This condition requires special attention due to its potential implications for both the expectant mother and the developing fetus. Understanding gestational diabetes and its impact on quality of life is essential in promoting better management and positive health outcomes. In this article, we delve into the intricacies of gestational diabetes, its prevalence, how it affects physical and emotional health, and why addressing the quality of life is crucial for those affected.
Brief Overview of Gestational Diabetes and Its Prevalence Among Pregnant Women
Gestational diabetes is a type of diabetes that only occurs during pregnancy. According to various studies, its prevalence varies widely, affecting approximately 5-10% of pregnancies globally, although this figure can be higher in certain populations and locations. As the incidence of obesity and sedentary lifestyles continues to rise, the prevalence of gestational diabetes is also expected to increase, making it a growing public health concern. The condition is typically diagnosed during the second trimester of pregnancy, through glucose screening tests.
- Definition and Diagnosis: GDM is defined as glucose intolerance, recognized first during pregnancy. Typically, it is diagnosed between the 24th and 28th weeks of pregnancy. Early detection is crucial for managing the condition effectively.
- Prevalence: The prevalence rates for GDM vary, with many studies suggesting higher rates in populations with ethnic and genetic predispositions, including South Asian, Hispanic, Native American, and African-American women. Factors such as obesity, advanced maternal age, and family history of diabetes also contribute to the risk.
- Rising Concerns: With increasing trends in obesity and lifestyle changes, gestational diabetes is becoming more common, necessitating heightened awareness and proactive management strategies.
Explanation of How Gestational Diabetes Affects Physical and Emotional Health
Gestational diabetes not only affects physical health but also has significant ramifications on emotional well-being. The period of pregnancy is already a time of substantial physical change, and the addition of a diabetes diagnosis can further strain a woman’s body and mind.
- Physical Health Effects:
- Maternal Risks: Women with gestational diabetes are at a higher risk for preeclampsia, a condition characterized by high blood pressure and potential organ damage. They are also more likely to require a cesarean section due to potential complications during delivery.
- Fetal Risks: Babies born to mothers with gestational diabetes may experience macrosomia, or being larger than average, which can complicate delivery. They are also at increased risk for neonatal hypoglycemia (low blood sugar) and later in life, obesity and type 2 diabetes.
- Emotional Health Effects:
- Anxiety and Stress: The diagnosis of gestational diabetes can lead to increased stress and anxiety over the health implications for both the mother and her baby. This stress is often compounded by dietary and lifestyle changes that are suddenly required.
- Impact on Self-perception: Women may feel a sense of guilt or inadequacy, fearing they might have contributed to the condition. This can impact their self-esteem and emotional health over the course of the pregnancy.
Managing gestational diabetes requires a multifaceted approach that addresses both physical and emotional aspects. Personalized care, nutritional counseling, and possibly medication are critical components of managing this condition effectively.
Importance of Addressing Quality of Life for Better Management and Health Outcomes
The quality of life for women with gestational diabetes is a vital area of focus for improving overall health outcomes. By addressing both the physical and emotional needs of these women, healthcare providers can offer more comprehensive care that benefits both mother and child.
- Comprehensive Care: Ensuring that women with GDM receive comprehensive care that addresses not just medical needs but also emotional support can profoundly improve their quality of life. Resources such as support groups and counseling play a significant role in this holistic approach.
- Education and Support: Educating mothers about gestational diabetes, its implications, and how to manage it effectively empowers them, reducing anxiety and enhancing their ability to adopt necessary lifestyle changes.
- Long-term Benefits: Focusing on quality of life has lasting benefits, potentially reducing the risk of developing type 2 diabetes later in life, both for the mother and the child. Monitoring and continued support post-pregnancy can also aid in maintaining a healthy lifestyle.
In conclusion, gestational diabetes is a health condition with significant implications for both mother and child. Understanding its prevalence, the impacts on physical and emotional health, and addressing the quality of life are paramount to managing this condition effectively. Providing comprehensive care and support ensures better health outcomes and creates a positive environment for both mother and child during this crucial phase of life.

2. The Role of Support Groups in Managing Gestational Diabetes
Gestational diabetes mellitus (GDM) is a condition characterized by high blood sugar levels that develop during pregnancy and typically resolve after giving birth. Managing gestational diabetes effectively is crucial not only for the health of the mother but also for the unborn child. While healthcare professionals provide the primary advice and medical treatment, support groups play an integral, often under-appreciated role in managing gestational diabetes by offering emotional backing and practical advice from those who have experienced the condition.
Definition and Types of Support Groups Available for Gestational Diabetes
Support groups are communities where individuals facing similar health challenges come together to share experiences, gather information, and support one another. For those managing gestational diabetes, these groups can become invaluable resources. Several types of support groups are accessible to individuals with gestational diabetes, including:
- In-Person Support Groups: These are commonly organized through hospitals, clinics, or community centers where pregnant women can meet regularly to discuss their experiences and share information.
- Online Support Communities: With the proliferation of social media and internet forums, online platforms such as Facebook groups, dedicated forums, and health-focused websites provide a space for individuals to connect from anywhere, breaking geographical barriers.
- Professional-Led Groups: Some support groups are moderated by healthcare professionals, providing a structured environment where participants can receive both emotional support and professional advice.
- Prenatal Classes: These classes often include segments that deal with managing gestational diabetes, offering a blended approach of information dissemination and peer support.
How Support Groups Provide Emotional Support and Practical Advice
The value of support groups in managing gestational diabetes extends beyond just peer support. They play an essential role in empowering women through:
- Emotional Support: Gestational diabetes can be an emotionally taxing condition as it involves lifestyle changes, strict monitoring, and the constant worry of affecting the baby’s health. Support groups offer a safe environment where individuals can express fears, anxiety, and frustrations, alleviating feelings of isolation.
- Sharing of Experiences: Hearing the stories and coping strategies of others who have successfully managed gestational diabetes can provide inspiration and hope, illustrating that the condition is controllable.
- Practical Advice: Members of support groups often share advice on meal planning, effective exercise routines, and blood sugar management techniques, all of which are crucial for managing gestational diabetes effectively.
- Access to Resources: Support groups can act as a conduit for additional resources, including educational materials, referrals to medical professionals, and information on local and online services.
Personal Testimonies or Case Studies Illustrating Positive Impacts of Support Groups
Real-life stories often resonate more strongly than statistics or generalized advice. Here are some personal testimonies and case studies that highlight the positive impacts of support groups for managing gestational diabetes:
- Case Study 1: Emily’s Journey:
Emily, a first-time mother, was diagnosed with gestational diabetes in her second trimester. Feeling overwhelmed by diet plans and glucose monitoring, she joined an online support group where she met other expecting mothers with gestational diabetes. The group provided a non-judgmental platform for sharing meal ideas and coping strategies. Emily attributes her ability to manage her blood sugar levels effectively to the consistent encouragement and tips she received from her online peers, easing her stress significantly. - Testimonial 2: Sarah’s Story:
Sarah attended a local prenatal class that combined regular sessions with a segment on managing gestational diabetes. The professional-led class wasn’t just informative; it also offered peer-led sessions where participants exchanged personal stories and useful lifestyle tips. Sarah felt better equipped to handle her condition, and the emotional validation she received became pivotal to her journey through pregnancy. - Testimonial 3: A Collective Experience:
A gestational diabetes support group organized at a regional hospital provided a unique blend of medical guidance and peer support. Expecting mothers shared weekly meetings where they could ask medical professionals questions and receive support from others experiencing the same challenges. One of the participants noted, “Understanding that I was not alone, especially when others shared their stories, gave me the strength to manage my health actively.”
These accounts exemplify the crucial role that support groups play in the lives of women diagnosed with gestational diabetes, transforming an overwhelming diagnosis into a manageable condition through communal strength and shared wisdom.
In conclusion, while gestational diabetes presents its challenges, support groups offer an effective strategy for managing this condition through emotional support and practical advice. Whether online or in-person, these communities provide invaluable resources, empowering individuals to take control of their health with confidence and solidarity.

3. Emotional and Psychological Benefits of Joining Support Groups
Gestational diabetes mellitus (GDM) is a condition that presents significant challenges not only physically but also emotionally and psychologically. For many, dealing with this condition can lead to increased stress, anxiety, and a myriad of mental health challenges. It’s essential to explore these challenges and understand how joining a support group can provide relief through community, shared experiences, and a sense of belonging.
Exploration of the Mental Health Challenges Faced by Individuals with Gestational Diabetes
Individuals diagnosed with gestational diabetes may often experience a range of emotions that can impact their mental health. Common challenges include:
- Anxiety: The health of both the mother and the baby becomes a predominant concern. Managing diabetes during pregnancy can lead to heightened levels of anxiety.
- Depression: The diagnosis may bring about feelings of inadequacy or concern about future health implications, contributing to depressive symptoms.
- Stress: The constant monitoring of blood sugar levels, dietary restrictions, and frequent doctor visits can lead to significant stress.
- Isolation: Feeling that others around them don’t understand what they’re experiencing can lead to a sense of loneliness.
Discussion on How Support Groups Offer a Sense of Community, Reducing Feelings of Isolation
One of the primary benefits of joining a support group is the creation of a community that understands and shares the challenges associated with gestational diabetes. This communal sense helps reduce feelings of isolation through:
- Connection: Meeting others who are experiencing or have experienced similar issues fosters a sense of belonging.
- Empathy and Understanding: In a support group, individuals find others who truly understand the fears and challenges they face.
- Supportive Environment: Support groups provide a non-judgmental space to express concerns and emotions freely.
When individuals feel connected to a community, the emotional burden of their condition often decreases, allowing them to better manage their mental health.
Importance of Shared Experiences in Alleviating Stress and Anxiety Related to the Condition
The power of shared experiences cannot be underestimated. Being part of a support group enables individuals with gestational diabetes to leverage the following benefits of shared experiences:
- Sharing Knowledge: Participants exchange tips and advice on managing their condition, contributing to collective wisdom.
- Emotional Relief: Articulating challenges and receiving validation from peers relieves pent-up stress and anxiety.
- Positive Role Models: Observing others who successfully manage their condition provides hope and motivation.
These groups often help participants develop coping strategies, promoting resilience and enhancing their overall sense of well-being. Support groups act as a vital tool in managing the psychological impact of gestational diabetes, providing essential emotional resources for overcoming the associated challenges.
4. Practical Advice and Information Sharing
Support groups play a pivotal role in managing gestational diabetes, providing a platform for expectant mothers to exchange practical advice and seek emotional solace. Gestational diabetes can often feel overwhelming; nevertheless, belonging to a community of individuals who share similar experiences can significantly alleviate this stress. An essential aspect of these groups is their ability to foster the sharing of effective tips and strategies that other members have found useful in managing the condition.
In these gatherings, it is paramount that the advice shared is evidence-based and endorsed by healthcare professionals, ensuring that the information is both safe and effective. A well-facilitated support group typically integrates expert contributions alongside peer sharing, resulting in a comprehensive support system.
Practical Tips and Strategies Shared in Support Groups
-
Dietary Recommendations: Nutrition is a critical element in controlling gestational diabetes. Support groups provide a platform for sharing dietary tips that have been successful for other expectant mothers. Sessions often include discussions on portion control, carb counting, and the inclusion of a balanced mix of proteins, fats, and carbohydrates. Real-life meal prepping strategies and recipes are frequently exchanged, providing practical insights applicable to daily life.
-
Exercise and Physical Activity: Exercise is another crucial component in managing gestational diabetes. Support groups delve into exercises that cater to different fitness levels and stages of pregnancy, from light walking routines to prenatal yoga. The sharing of how others have safely incorporated physical activities into their routines often inspires and motivates members to remain active.
-
Medication and Monitoring: The use of medications like insulin may be necessary for some, and support groups often address concerns and strategies related to medication adherence. Discussions typically include practical tips on maintaining glucose monitoring logs and interpreting blood sugar readings.
The Role of Healthcare Professionals in Support Groups
To ensure the information disseminated in support groups is accurate and reliable, the integration of healthcare professionals is indispensable. Their presence guarantees that the advice given is grounded in medical evidence, allowing them to correct misconceptions and guide discussions to be both informative and safe.
-
Facilitating Evidence-based Discussions: Healthcare professionals can direct conversations towards proven strategies and dispel myths that may circulate within community settings. Their clinical knowledge equips them to explain the complex nature of gestational diabetes, enhancing members’ understanding of the condition.
-
Providing Personalized Feedback: Within the support group context, professionals can offer tailored advice in a public yet personalized manner. This dual approach allows members to learn from others’ experiences while also receiving guidance pertinent to their unique circumstances.
-
Staying Updated with Current Research: The field of diabetes management is continuously evolving, and support groups led by informed healthcare providers serve as conduits for sharing the latest research and guidelines. This ensures members have access to contemporaneous advice on managing gestational diabetes.
Examples of Topics Covered in Support Group Sessions
Support groups for gestational diabetes cover a broad range of topics, each tailored to empower participants with the knowledge and skills needed to effectively manage their condition. Some of the prevalent themes include:
-
Understanding Gestational Diabetes and Its Implications: Many support groups dedicate sessions to educating members about what gestational diabetes is, its potential impacts on both mother and baby, and the importance of effective management.
-
Meal Planning and Cooking Demonstrations: Interactive workshops that involve meal planning and cooking demonstrations can help demystify nutritional guidelines and allow expectant mothers to learn practical skills to implement at home.
-
Stress Management Techniques: Gestational diabetes can be a significant source of stress. Support groups often explore strategies such as mindfulness, meditation, or relaxation techniques to help manage anxiety and promote overall well-being.
-
Preparing for Labor and Delivery: Sessions may include discussions on how gestational diabetes can affect labor and delivery, as well as preparation tips for a healthy birthing experience.
In summary, support groups provide an invaluable resource for expectant mothers grappling with gestational diabetes by facilitating the sharing of practical advice, fostering community support, and promoting evidence-based strategies. By offering sessions on crucial topics such as diet, exercise, and medication, and with the guidance of healthcare professionals, these groups empower women to manage their health effectively through pregnancy and beyond.