Innovative Technologies Changing the Game for Diabetic Management
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Innovations in Diabetic Management
Diabetes, a chronic condition characterized by high blood sugar levels, is becoming increasingly prevalent across the globe, affecting millions of people and posing significant public health challenges. Understanding and managing diabetes effectively is crucial, as it can lead to serious health complications such as heart disease, kidney failure, and nerve damage if left uncontrolled. This growing concern has driven the need for creative and innovative approaches in diabetic management to enhance patient outcomes and improve quality of life.
In recent decades, the landscape of diabetic care has been transformed by technological advancements and innovative practices. These innovations are not only crucial for personalizing care and improving efficiency but also for reducing healthcare costs and minimizing the burden on healthcare systems. To truly appreciate the contributions of these technologies, it’s important to understand the global context and appreciate the significance of these developments within the broader scope of diabetic care.
- Rising Prevalence of Diabetes Globally:
Diabetes is no longer just a regional concern; it has become a global epidemic. Data from the International Diabetes Federation indicates a staggering increase in the prevalence of the disease, with current projections suggesting that nearly 700 million adults will be affected by 2045. Various factors contribute to this alarming trend, including lifestyle changes, aging populations, and genetic predispositions. These statistics highlight the urgency in developing more effective strategies to tackle the diabetes crisis.
- Importance of Innovative Technologies in Improving Diabetic Care:
Technological innovation in diabetic management offers hope for reversing the growing trend of the disease’s prevalence. Cutting-edge technologies such as continuous glucose monitors, insulin pumps, and artificial pancreas systems have revolutionized how diabetes is managed, providing patients with tools to track their condition in real-time and adjust their treatment regimens accordingly. These technologies not only enhance accuracy and convenience but also empower patients to take control of their health.
- Objectives Covered in the Article:
The dynamic landscape of diabetes care necessitates a comprehensive exploration of these technological advancements. In this article, we will delve into the latest innovations in diabetic management, examining how they are transforming care delivery. We will:
- Provide an in-depth analysis of the most promising technological advancements in diabetic care.
- Explore the role of digital health tools and data analytics in personalizing treatment plans.
- Discuss the impact of these innovations on patient-centric care and self-management.
- Highlight future trends and emerging technologies in diabetes management.
Addressing diabetes effectively requires a multifaceted approach that combines advanced technology with practical care strategies. As we continue to witness the rapid evolution of diabetic management techniques, it is crucial to stay informed about these developments and understand their implications for both healthcare providers and patients worldwide. Through embracing innovation, we can improve diabetes care delivery and ultimately strive for better health outcomes for those affected by this pervasive condition.

2. Continuous Glucose Monitoring Systems (CGMs)
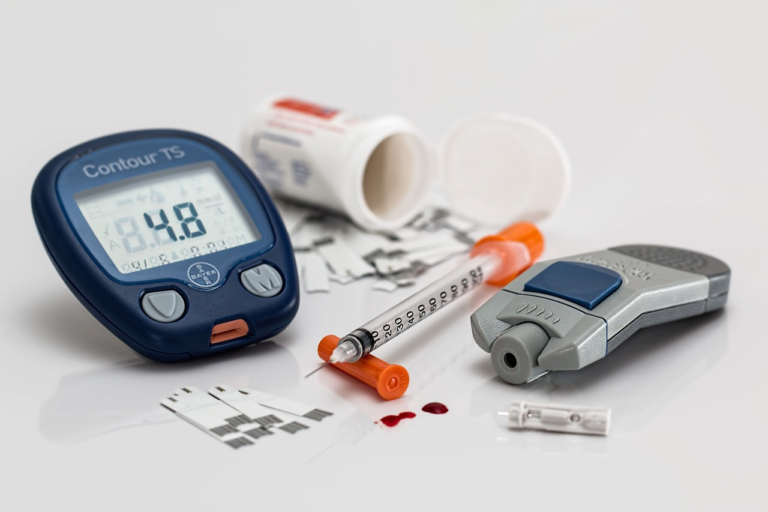
Continuous Glucose Monitoring Systems (CGMs) represent a significant advancement in the management of diabetes. These devices have revolutionized the way individuals monitor their glucose levels, offering more comprehensive data and insights compared to traditional methods like finger-prick tests. Understanding how CGMs work and recognizing their benefits is crucial for both healthcare providers and patients seeking improved diabetic management.
Explanation of How CGMs Work and Their Benefits Over Traditional Methods
CGMs are wearable devices that provide real-time feedback about glucose levels. They work by using a small sensor inserted under the skin, typically on the abdomen or arm, which measures interstitial glucose levels — the sugar level in the fluid between cells. These readings are taken automatically at regular intervals, typically every few minutes, and sent to a display device, such as a smartphone or a dedicated monitor. Unlike traditional methods, CGMs offer continuous data, minimizing the need for frequent finger-prick tests.
- Real-Time Glucose Monitoring: CGMs provide dynamic glucose readings, alerting users to rising or falling trends that need immediate attention.
- Reduce Hypoglycemia Risk: Continuous monitoring helps in reducing the risk of hypoglycemia by alerting users well before glucose levels drop too low.
- Data for Health Decisions: The extensive data collected helps in making informed decisions regarding diet, exercise, and medication, allowing for personalized diabetic management.
- Enhanced Lifestyle Flexibility: Users have more freedom in their daily lives without the constant need to conduct finger-stick tests.
Key Features of the Latest CGMs and Their Impact on Daily Diabetic Management
The latest models of CGMs come equipped with advanced features, making them even more beneficial to users. These enhancements not only improve the accuracy of glucose readings but also integrate seamlessly with modern technology solutions to provide a holistic approach to diabetes management.
- Improved Sensor Technology: Latest CGMs have sensors with increased accuracy and longevity, often lasting up to 14 days per sensor.
- Smartphone Integration: Many CGMs can connect directly to smartphones, allowing users to not only monitor their glucose levels but also share the data with healthcare providers instantly.
- Predictive Alerts: Advanced algorithms inCGMs provide predictive alerts, helping users take precautionary actions before hypo- or hyperglycemic episodes.
- Data Analysis Tools: Users have access to comprehensive data analysis tools that help in detecting patterns and adjusting their lifestyle and treatment plans accordingly.
- Personalized Recommendations: Some CGMs now offer personalized insights and recommendations based on individual glucose patterns and lifestyle habits.
Overall, the integration of these features ensures better glucose control, reduced risk of complications, and an improved quality of life for individuals with diabetes.
Case Studies or Statistics Showcasing Improvements in Patient Outcomes
To further illustrate the impact of CGMs on diabetic management, let’s delve into specific case studies and statistical data that highlight the benefits observed in patient outcomes through the use of CGMs.
- Improved Glycemic Control: A study published in the Journal of Clinical Endocrinology & Metabolism reported that patients using CGMs experienced a significant reduction in HbA1c levels by an average of 1% compared to those using traditional monitoring methods.
- Reduction in Hypoglycemic Episodes: A clinical trial indicated a 40% reduction in hypoglycemic episodes among patients who utilized CGM technology, showcasing its effectiveness in maintaining stable blood glucose levels.
- Positive Behavioral Changes: In a survey conducted among CGM users, 75% of participants reported making positive lifestyle adjustments as a direct result of real-time glucose data, leading to healthier living.
- Enhanced Patient Engagement and Satisfaction: According to a study published in Diabetes Technology & Therapeutics, 93% of CGM users expressed increased satisfaction with their diabetes management regimen, mainly due to the ease of tracking glucose levels and the reduced dependency on manual testing.
These case studies underscore the profound impact CGMs have had on improving the management and treatment of diabetes, providing invaluable support and data that enable both patients and healthcare professionals to make more informed decisions.

3. Artificial Intelligence and Machine Learning in Diabetes Care
In recent years, the integration of artificial intelligence (AI) and machine learning (ML) in healthcare has revolutionized various aspects of patient care, including the management of chronic conditions like diabetes. By leveraging the power of AI-driven tools, healthcare professionals can now offer personalized diabetes management to patients, enhancing their quality of life and optimizing treatment outcomes.
Description of AI-driven Tools for Personalized Diabetes Management
AI-driven tools have become indispensable in the fight against diabetes, providing tailored treatment plans and real-time monitoring systems. Personalized diabetes management approaches utilize vast amounts of data collected from patients to deliver individualized care. These tools can analyze glucose levels, food intake, physical activity, and medication adherence, enabling healthcare providers to develop customized treatment strategies.
- Continuous Glucose Monitoring (CGM): AI-enhanced CGMs are equipped with sensors that track glucose levels 24/7. By analyzing this data, these systems can predict blood sugar fluctuations, alerting patients of potential hypo- or hyperglycemia.
- Smart Insulin Pens: These devices use AI to recommend insulin doses based on an individual’s current glucose level, dietary intake, and previous insulin usage, reducing the risk of errors in dosage calculations.
- Digital Therapeutics: AI-powered digital platforms offer personalized recommendations and support for lifestyle changes, such as diet and exercise, aligning with a patient’s unique needs and preferences.
The Role of Predictive Analytics in Forecasting Blood Sugar Trends
One of the most notable advancements brought by AI and ML in diabetes care is the use of predictive analytics. By deploying sophisticated algorithms, predictive analytics can forecast blood sugar trends with remarkable accuracy. This enables patients to anticipate potential spikes or dips in glucose levels, affording them greater control over their condition.
- Pattern Recognition: AI systems can identify patterns in blood sugar levels by analyzing historical data. This pattern recognition is crucial for predicting future glucose trends and adjusting treatment plans accordingly.
- Real-Time Decision Support: Predictive analytics provide real-time decision support by analyzing the impact of different factors such as meals, activities, and medication adherence on glucose levels, allowing for immediate adjustments.
- Preventive Measures: By forecasting potential deviations in blood sugar levels, AI-driven predictive analytics facilitate timely interventions, reducing the risk of complications associated with diabetes.
Example Applications and Emerging Startups in this Space
The burgeoning field of AI and ML in diabetes management has encouraged the development of innovative applications and the emergence of startups dedicated to enhancing diabetes care. Here are a few notable examples:
- Glooko: A dynamic platform offering diabetes data management by syncing with devices like CGMs, insulin pumps, and fitness trackers. It employs AI to provide insights, reports, and personalized recommendations.
- Virta Health: A cutting-edge startup focusing on reversing type 2 diabetes through a combination of personalized medical advice and technology-driven nutrition plans.
- PredictBGL: A sophisticated diabetes management app that uses advanced mathematics and AI to predict blood glucose levels, suggesting insulin, carbs, and activities to maintain balance.
- Sugar.IQ: Powered by IBM Watson, this app offers real-time glucose insights and personalized diabetes management support, helping patients avoid potential blood sugar issues.
These AI-driven tools and startups showcase the immense potential of artificial intelligence and machine learning in transforming diabetes care. By leveraging predictive analytics and personalized solutions, they empower both patients and healthcare providers, driving a new era of diabetes management where proactive care and improved outcomes are at the forefront.
In conclusion, the continual advancement of AI and ML technologies in diabetes management promises further enhancements in patient care. As these tools become more sophisticated, we can expect even greater levels of personalization, predictive accuracy, and integration into daily life, all contributing to a healthier future for individuals managing diabetes.
4. Smartphone Apps and Digital Platforms
In today’s fast-paced digital era, managing health conditions like diabetes has become more convenient, thanks to the proliferation of smartphone apps and digital platforms. These tools are instrumental in diabetes monitoring and lifestyle management, empowering individuals to take charge of their health with unprecedented ease.
Overview of Mobile Apps Designed for Diabetes Monitoring and Lifestyle Management
Mobile apps serve as a vital resource for those living with diabetes, offering features that can track blood glucose levels, monitor dietary intake, and even remind users to take their medications. The following are key aspects that highlight the functionality and benefits of these apps:
- Blood Glucose Monitoring: Many apps allow users to log and track their blood glucose levels, providing a visual representation of fluctuations over time. This feature helps individuals understand their body’s response to various foods and activities.
- Diet and Nutrition Tracking: Apps often include food diaries or barcode scanners to simplify tracking dietary intake. They also provide nutritional information to help users make informed dietary choices.
- Medication Reminders: To ensure medication adherence, apps can generate alerts for upcoming doses, thus preventing missed medications.
- Activity and Exercise Tracking: Regular exercise is crucial for diabetes management, and many apps sync with fitness trackers to log physical activity and progress towards fitness goals.
- Educational Resources: Some apps provide access to educational materials, tips, and community support to help users stay informed about their condition and treatment options.
Integration with Other Devices and Platforms for Seamless Data Tracking
The integration of diabetes apps with other devices and platforms has significantly enhanced data accuracy and user convenience. The synergy between apps and external devices like continuous glucose monitors (CGMs) or smart insulin pens provides a more comprehensive overview of a user’s health. Here’s a look at how these integrations are helping:
- Continuous Glucose Monitors: Apps that connect with CGMs receive real-time data on blood glucose levels, facilitating immediate insights and timely interventions.
- Smart Insulin Pens: When integrated with apps, these pens can transmit information about insulin doses, offering a complete view of insulin management.
- Wearable Fitness Devices: Syncing with fitness trackers allows apps to log exercise details such as steps, heart rate, and calories burned, fostering a holistic approach to diabetes management.
- Cloud-Based Data Storage: Integration with cloud platforms enables data synchronization across devices, ensuring that health information is easily accessible from smartphones, tablets, and desktops.
User Testimonials and Expert Opinions on Effective App-Based Management
The effectiveness of diabetes management apps is evident in numerous user testimonials and expert analyses. Users have shared transformative experiences, revealing how these digital solutions have improved their daily lives and overall health outcomes.
- “The app’s glucose tracking feature has been a lifesaver for me. I no longer have to jot down numbers manually, and the trend analysis really helps me understand my patterns better.” – John D., App User
- “Integrating my fitness tracker with the diabetes app has motivated me to stay more active. I now have a clear record of how exercise affects my glucose levels.” – Sarah P., App User
Experts also lend their voices, emphasizing the impact of technology on diabetes management. Dr. Emily Roberts, an endocrinologist, remarks:
“The advent of digital health solutions, particularly mobile apps, marks a significant advancement in diabetes care. These tools offer personalized data management, enabling patients to achieve better glycemic control.” – Dr. Emily Roberts
In conclusion, smartphone apps and digital platforms have revolutionized diabetes management by offering robust features that cater to individual needs. Through seamless integration with various devices, these apps provide comprehensive data tracking and foster better lifestyle choices. The positive feedback from users and experts solidifies the role of app-based management as a cornerstone in the ongoing battle against diabetes.