The Impact of Sleep on Blood Glucose Levels in Diabetic Patients
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to the Relationship Between Sleep and Diabetes
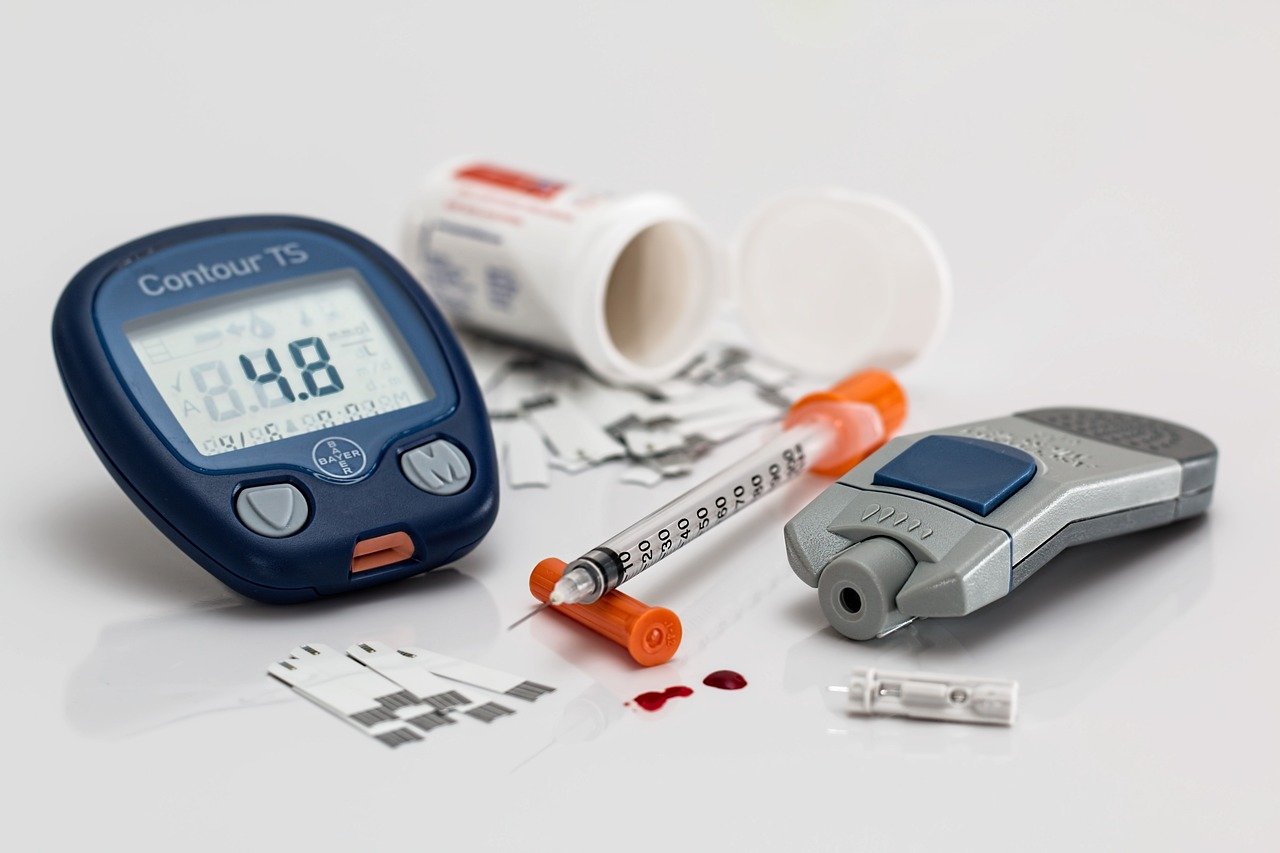
Diabetes is a chronic condition that affects millions of people worldwide, characterized by high levels of sugar in the blood. Understanding the relationship between sleep and diabetes is crucial for managing and preventing this condition. In this article, we will delve into how sleep impacts diabetes and why prioritizing sleep is essential for overall health.
Overview of Diabetes and Its Prevalence
Diabetes is primarily categorized into two types: Type 1 and Type 2.
- Type 1 Diabetes: An autoimmune condition where the body’s immune system attacks insulin-producing cells in the pancreas.
- Type 2 Diabetes: A metabolic disorder often linked to obesity and lifestyle, where the body becomes resistant to insulin.
Statistics reveal an alarming rise in diabetes prevalence:
- As of the latest reports, over 420 million people globally are living with diabetes.
- The prevalence has doubled in the past four decades, with Type 2 diabetes accounting for the majority of cases.
Importance of Sleep in Overall Health
Sleep is vital for maintaining physical and mental health. It influences various bodily functions, including:
- Cognitive Function: Adequate sleep enhances memory, learning, and problem-solving skills.
- Physical Health: Sleep is essential for repairing muscles, tissues, and promoting growth, particularly in children and teens.
- Emotional Well-being: Proper sleep helps regulate mood and manage stress levels, reducing the risk of depression and anxiety.
Poor sleep is linked to numerous health issues, such as cardiovascular diseases, obesity, and weakened immune function. Therefore, understanding its impact on diabetes is imperative.
Brief Introduction to the Connection Between Sleep and Blood Glucose Levels
The relationship between sleep and diabetes primarily revolves around how sleep affects blood glucose levels:
- Insulin Sensitivity: Insufficient sleep has been shown to decrease insulin sensitivity, leading to elevated blood glucose levels.
- Glucose Metabolism: Sleep deprivation disrupts the body’s ability to process glucose efficiently, increasing the risk of Type 2 diabetes.
- Hormonal Balance: Lack of sleep affects hormones that regulate appetite, increasing cravings for sugary foods and contributing to poor blood sugar management.
Emerging research suggests a bi-directional relationship between sleep and diabetes, where managing sleep can positively impact blood glucose regulation, and stable glucose levels can improve sleep quality.
Understanding these connections is the first step towards leveraging sleep as an integral part of diabetes management.

2. Understanding Blood Glucose Levels and Their Significance in Diabetes Management
Understanding blood glucose levels is pivotal for effective diabetes management. This segment will delve into blood glucose’s crucial role in the body, how it is regulated in both non-diabetic and diabetic individuals, and the immense importance of maintaining stable blood glucose levels for those managing diabetes.
Explanation of Blood Glucose and Its Role in the Body
Blood glucose, often referred to as blood sugar, is the primary sugar found in your blood. It originates from the food you consume and serves as a vital energy source for your body’s cells. The glucose journey in your body can be summarized as follows:
- Energy Production: Blood glucose is essential for generating energy. Cells use glucose to perform various functions, from muscle contractions to nerve signaling.
- Brain Function: The brain is especially dependent on glucose. It uses more glucose than any other organ in the body, which highlights the importance of steady blood glucose levels for cognitive functions.
- Metabolism Regulation: Glucose acts as a metric by which your body gauges its energy reserves. It influences how other metabolic processes, like fat and protein breakdown, are conducted.
How Blood Glucose Levels Are Regulated
The regulation of blood glucose levels is a complex system primarily managed by hormones. Understanding how this regulation differs between non-diabetic and diabetic individuals is crucial:
In Non-Diabetic Individuals
In individuals without diabetes, blood glucose levels are tightly regulated by a series of coordinated events:
- Insulin Release: After consuming food, blood glucose levels rise, prompting the pancreas to release insulin. Insulin is a key hormone that facilitates the entry of glucose into cells for energy.
- Glucose Storage: Excess glucose is stored in the liver in the form of glycogen. When blood glucose levels drop, glycogen is converted back to glucose to maintain balance.
- Hormonal Balance: Alongside insulin, glucagon and other hormones also work to stabilize blood glucose levels during fasting periods or physical activity.
In Diabetic Individuals
In those with diabetes, the regulation of blood glucose levels is impaired, leading to persistent high blood sugar levels (hyperglycemia) or, in some cases, low blood sugar (hypoglycemia):
- Type 1 Diabetes: The body’s immune system attacks insulin-producing cells, resulting in little or no insulin production.
- Type 2 Diabetes: Cells become resistant to insulin, and there is an eventual decline in insulin production.
- Gestational Diabetes: Pregnancy hormones can affect the body’s ability to use insulin efficiently, leading to temporary glucose regulation issues.
The Importance of Maintaining Stable Blood Glucose Levels for Diabetic Patients
For individuals managing diabetes, maintaining stable blood glucose levels is crucial to avoid complications associated with fluctuating blood sugar levels:
- Prevention of Complications: Chronic high blood glucose can lead to complications such as retinopathy, neuropathy, and cardiovascular diseases.
- Improved Quality of Life: Stable glucose levels can help diabetic individuals maintain a better quality of life, reducing the risk of hospitalization and the burden of daily management.
- Long-term Health Benefits: Maintaining optimal glucose levels can greatly reduce the risk of complications, contributing to increased longevity.
Achieving stable blood glucose levels often involves a combination of medication, regular monitoring, a balanced diet, and physical activity. Tailored plans by healthcare providers can help patients get the best possible outcomes in diabetes management.
Ultimately, understanding blood glucose levels and their role in the body, as well as implementing strategies to maintain these levels, is integral to effective diabetes management. Through diligent management, individuals with diabetes can lead healthy, fulfilling lives.

3. The Role of Sleep in Regulating Blood Glucose Levels
Sleep, an often-overlooked aspect of health, plays a significant role in the regulation of blood glucose levels. Understanding the intricate relationship between sleep quality, sleep duration, and glucose metabolism can shed light on the importance of adequate rest for effective blood sugar control. This article provides an in-depth analysis of the role of sleep in managing blood glucose levels, supported by scientific studies and an explanation of how sleep deprivation affects insulin sensitivity.
Quality and Duration of Sleep and Their Effect on Blood Glucose Control
Both the quality and duration of sleep significantly impact blood glucose levels. Quality sleep refers to a restful sleep with reduced awakenings and a proper progression through the sleep cycles, which helps in the regulation of hormones crucial for glucose metabolism. Conversely, sleep duration pertains to the amount of sleep one gets. Both aspects are essential in maintaining healthy blood glucose levels.
-
Quality of Sleep: Poor sleep quality can lead to hormonal imbalances that adversely affect glucose regulation. For instance, inadequate deep sleep stages can decrease insulin sensitivity, increasing the risk of higher blood sugar levels.
- Deep sleep stages, particularly slow-wave sleep, are crucial for repairing and rejuvenating the body, including the endocrine systems managing glucose.
- Interruptions during sleep can result in elevated cortisol levels, a stress hormone that can increase blood glucose levels.
-
Duration of Sleep: Short or prolonged sleep durations have been linked to impaired glucose metabolism. Optimal sleep typically ranges between 7 to 9 hours per night for most adults.
- Short sleep durations, defined as less than 6 hours per night, are associated with increased insulin resistance.
- Excessive sleep, more than 9 hours, can also have detrimental effects on glucose metabolism, albeit for reasons that are still being studied.
Scientific Studies Linking Sleep Patterns with Glucose Metabolism
Several scientific studies have explored the connection between sleep patterns and glucose metabolism, further strengthening the claim that sleep is an integral component of glycemic control. Below is a summary of key findings from various research endeavors.
-
Study on Sleep Restriction: A study conducted by the Centers for Disease Control and Prevention found that short-term sleep restriction resulted in a significant decrease in insulin sensitivity, which is a precursor to type 2 diabetes.
- Participants who had restricted sleep for just a few days showed a marked increase in insulin resistance.
- This study underscores the impact of acute sleep deprivation on blood glucose levels and indicates the potential for long-term consequences.
-
Circadian Rhythm Studies: Research published in the Journal of Clinical Endocrinology & Metabolism suggests that disruptions in circadian rhythms negatively influence glucose metabolism.
- The body’s internal clock regulates hormones such as insulin, and disturbances can lead to impaired glucose tolerance.
- Shift workers or those with irregular sleep patterns are often at higher risk for metabolic syndromes due to circadian misalignment.
Sleep Deprivation and Its Impact on Insulin Sensitivity
Sleep deprivation is a growing concern, particularly in today’s fast-paced world. Its impact on insulin sensitivity is profound and multifaceted, affecting the body’s ability to efficiently process glucose. Understanding these impacts helps in formulating strategies to mitigate the risks associated with insufficient sleep.
-
Increased Hunger Hormones: Sleep deprivation elevates levels of ghrelin, the hormone that increases hunger, while reducing leptin, the hormone responsible for satiety.
- This imbalance can lead to increased calorie intake and weight gain, which are risk factors for insulin resistance.
- Snacking on high-carb foods may become more tempting, leading to erratic blood sugar levels.
-
Inflammatory Responses: Chronic sleep deprivation can initiate an inflammatory response in the body that negatively affects insulin action.
- Prolonged inflammation can damage insulin receptors and reduce their ability to function properly, directly impacting glucose uptake in cells.
- Inflammatory cytokines such as TNF-alpha and IL-6 are often elevated in individuals with poor sleep, correlating with decreased insulin sensitivity.
The scientific community continues to unravel the complexities between sleep and blood glucose regulation, yet it’s clear that maintaining good sleep hygiene is a crucial element in controlling blood sugar levels effectively. By ensuring adequate rest, individuals can potentially reduce their risk of developing insulin resistance and, ultimately, type 2 diabetes.
If we prioritize quality sleep as part of a comprehensive lifestyle change, alongside a balanced diet and regular exercise, the prospects for maintaining healthy blood glucose levels improve significantly. As such, healthcare providers are increasingly recognizing and advocating for better sleep management as part of diabetes prevention and management strategies.
4. Strategies for Improving Sleep Quality in Diabetic Patients
Quality sleep is fundamental for everyone, yet individuals with diabetes often face unique challenges when it comes to achieving restful sleep. Improving sleep quality in diabetic patients requires a comprehensive approach, blending various strategies and lifestyle modifications. This segment explores vital tips and lifestyle adjustments that can enhance sleep quality, the critical role of sleep hygiene in diabetes management, and a discussion on the use of sleep aids and alternative therapies.
Tips and Lifestyle Changes to Enhance Sleep Quality
Improving sleep quality begins with making certain changes to daily habits and routines. Here are some effective strategies:
- Maintain a Consistent Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends. This helps regulate the body’s internal clock.
- Create a Relaxing Bedtime Ritual: Engage in calming activities before bed, such as reading, listening to soothing music, or practicing meditation.
- Watch Your Diet: Avoid heavy meals, caffeine, and alcohol in the hours leading up to bedtime as they can disrupt sleep.
- Exercise Regularly: Physical activity can help you fall asleep faster and enjoy deeper sleep. However, avoid vigorous exercise close to bedtime.
- Limit Daytime Naps: While naps can be beneficial, limit them to 30 minutes and avoid napping late in the afternoon.
These changes not only improve sleep quality but also positively affect diabetes management, as good sleep is linked to better blood sugar control.
The Role of Sleep Hygiene and Its Impact on Diabetes Management
Sleep hygiene refers to the environmental and behavioral practices that promote restful sleep. It plays a crucial role in diabetes management by influencing factors such as insulin sensitivity and blood sugar levels. Here’s how you can enhance sleep hygiene:
- Create a Comfortable Sleep Environment: Ensure your bedroom is conducive to sleep—it’s quiet, dark, and cool. Consider using blackout curtains or a white noise machine if necessary.
- Avoid Electronics Before Bedtime: The blue light emitted by phones, tablets, and computers can interfere with your body’s preparation for sleep.
- Invest in a Good Mattress and Pillow: Your bed should support your body well and feel comfortable. This helps prevent aches and pains that can interrupt sleep.
- Establish a Pre-Sleep Routine: Train your body to recognize cues that it’s time to sleep by engaging in the same pre-bedtime activities each night.
The impact of sleep hygiene on diabetes management cannot be overstated. Consistently poor sleep can exacerbate insulin resistance and contribute to unstable blood sugar levels, making sleep hygiene a vital component of effective diabetes care.
Discussion on the Use of Sleep Aids and Alternative Therapies
While lifestyle changes and sleep hygiene are key strategies, some diabetic patients may still struggle with sleep disorders and might consider sleep aids or alternative therapies. Here’s a discussion on these options:
- Over-the-Counter (OTC) Sleep Aids: Commonly contain antihistamines. They can be effective for occasional sleeplessness but are not recommended for long-term use due to potential side effects.
- Prescription Sleep Medications: These can be more effective for chronic insomnia but should be used under the guidance of a healthcare professional.
- Melatonin Supplements: A natural sleep aid that can help regulate sleep cycles, particularly beneficial for those experiencing issues due to shift work or jet lag.
- Alternative Therapies: Practices such as acupuncture, cognitive behavioral therapy for insomnia (CBT-I), and aromatherapy with essential oils like lavender can offer non-pharmacological solutions.
While exploring sleep aids, it’s crucial for diabetic patients to consult with their healthcare providers, as some medications can impact blood sugar levels or interact with diabetes medications.
In conclusion, enhancing sleep quality in diabetic patients involves more than just addressing sleep itself. It requires an integrated approach involving lifestyle modifications, maintaining good sleep hygiene, and carefully considering the use of sleep aids or alternative therapies. By prioritizing restful sleep, diabetic individuals can significantly improve their overall health and diabetes management.