The Role Of Mindfulness In Managing Blood Sugar Levels For Diabetics
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Mindfulness and Diabetes
Introduction to Mindfulness and Diabetes
The journey of managing diabetes is not just a physical endeavor but an emotional and psychological one as well. With growing awareness of holistic health, mindfulness has emerged as a key practice in enhancing overall well-being, especially for individuals living with diabetes. This piece aims to explore the dynamic interplay between mindfulness and effective diabetes management, providing insights into how these practices can significantly benefit those managing the condition.
- Definition and Overview of Mindfulness Practices
Mindfulness is a mental state achieved by focusing one’s awareness on the present moment, while calmly acknowledging and accepting one’s feelings, thoughts, and bodily sensations. It is a form of meditation that prioritizes consciousness and attention, allowing individuals to resiliently navigate the complexities of daily life.
Mindfulness practices can be easily integrated into daily routines. These practices include:
- Breathing Exercises: Paying attention to the breath to anchor oneself in the present moment.
- Body Scan: A mindful practice of scanning the body to release any tension.
- Mindful Eating: Engaging fully in the dining experience without distractions, focusing on the taste, texture, and aroma of food.
- Mindful Walking: Observing the movement of one’s body and nature during a walk.
- Guided Meditation: Listening to a narration or ambient sounds to facilitate relaxation and mindfulness.
Practicing mindfulness not only alleviates stress and anxiety but also nurtures a deeper connection within oneself, fostering an environment conducive to better emotional and physical health.
- Brief Explanation of Diabetes and the Importance of Blood Sugar Management
Diabetes is a chronic condition characterized by high levels of sugar (glucose) in the blood. This happens when the body’s ability to produce or respond to the hormone insulin is impaired. Broadly, diabetes is categorized into two main types:
- Type 1 Diabetes: An autoimmune disorder where the body’s immune system attacks insulin-producing cells in the pancreas.
- Type 2 Diabetes: A metabolic condition that arises when the body becomes resistant to insulin or when the pancreas fails to produce enough insulin.
The management of diabetes primarily revolves around maintaining healthy blood sugar levels to prevent complications that can lead to damage in various organs and tissues, including the heart, kidneys, eyes, and nerves. Effective blood sugar management involves:
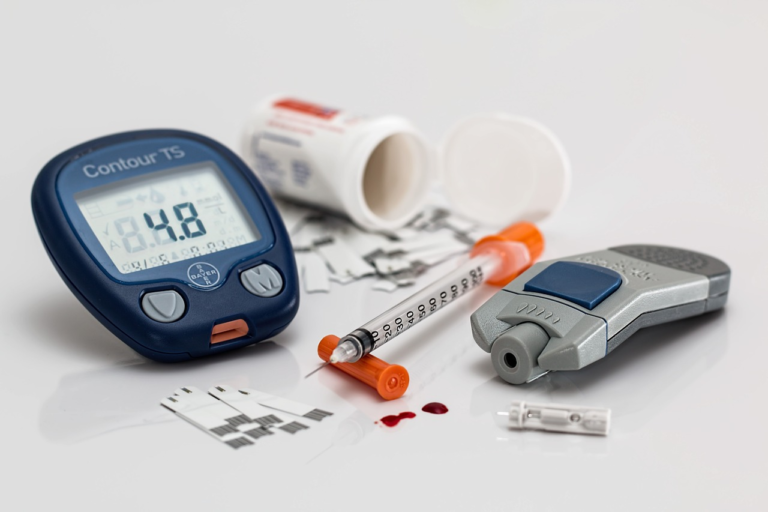
- Regular monitoring of blood glucose levels.
- Adhering to a balanced diet rich in whole foods.
- Regular physical activity to support insulin sensitivity.
- Adhering to medication regimens as prescribed by healthcare professionals.
- Stress management techniques to prevent spikes in blood sugar.
The interplay of physical and emotional factors makes it essential to adopt a comprehensive approach, targeting both the physical symptoms and emotional triggers associated with diabetes.
- Connection between Mindfulness and its Potential Impact on Diabetes Management
Incorporating mindfulness into diabetes management can unlock a plethora of benefits. Research has shown that mindfulness practices can significantly improve various aspects of diabetes care:
- Enhanced Blood Sugar Control: By reducing stress and promoting emotional balance, mindfulness practices can positively influence blood glucose levels. Stress hormones like cortisol can raise blood sugar levels, and mindfulness practices help in mitigating these effects.
- Improved Dietary Choices: Mindful eating can lead to healthier food selections and portion control, contributing to better glucose management.
- Stress Reduction: Mindfulness aids in stress reduction, curtailing its negative effects on blood sugar and promoting a state of calm that assists people in making thoughtful health decisions.
- Emotional Regulation: Better control over emotions and mood swings, often influenced by fluctuating blood sugar levels, can be achieved through mindfulness training.
- Increased Physical Activity: Mindfulness can encourage a conscious approach to exercise, enhancing motivation and enjoyment of physical activities which in turn help in managing blood sugar levels.
The incorporation of mindfulness offers a unique intersection of mental and physical health, providing a holistic framework to aid in diabetes management. It emphasizes the body’s intrinsic capability to restore and regulate itself, equipping individuals with the tools needed to live a balanced and fulfilling life despite the challenges posed by diabetes.
In essence, mindfulness paves the way for mindful living, where individuals with diabetes are empowered to cultivate inner peace, enhance their emotional intelligence, and nurture self-compassion, paving the path towards effective diabetes management and overall well-being.

2. Understanding Blood Sugar Levels and Their Significance
Understanding blood sugar levels is crucial for grasping their impact on diabetic patients. These levels are indicative of the amount of glucose present in the bloodstream at any given time. Glucose, a fundamental energy source, is essential for bodily functions; however, maintaining its optimal levels becomes critical, particularly for individuals diagnosed with diabetes.
-
Explanation of Blood Sugar Levels and Their Impact on Diabetic Patients
Blood sugar levels, also known as blood glucose levels, represent the concentration of glucose in a person’s blood. Typically, they are measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). For most non-diabetic individuals, fasting blood sugar levels range from 70 to 99 mg/dL.
For diabetic patients, managing blood sugar is vital to avoid both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). Hyperglycemia can lead to long-term complications such as heart disease, kidney damage, and vision problems. Conversely, hypoglycemia can cause immediate dangers like dizziness, confusion, or even loss of consciousness.
-
The Role of Blood Sugar Monitoring in Diabetes Care
Monitoring blood sugar levels is a cornerstone of effective diabetes management. This practice enables patients and healthcare providers to understand how various factors like diet, exercise, medication, and stress affect blood glucose levels. Regular monitoring helps in making informed decisions about lifestyle and treatment adjustments, aiming to maintain levels within recommended targets.
Diabetes care often includes tools such as:
- Continuous Glucose Monitors (CGMs): Devices that provide real-time glucose level data, alerting users to rising or falling levels.
- Glucometers: Portable devices used to test blood sugar levels at specific intervals by analyzing a drop of blood.
-
Common Challenges Diabetics Face in Maintaining Stable Blood Sugar Levels
The journey to stabilize blood sugar levels is fraught with challenges, often unique to each individual. Some common hurdles include:
-
Dietary Management
Choosing the right foods and understanding their impact on blood sugar levels can be difficult. Carbohydrates, particularly refined sugars, require careful monitoring as they can cause spikes in blood glucose levels.
-
Physical Activity
While exercise is beneficial, it affects blood sugar differently for everyone. Finding the right balance to prevent exercise-induced hypoglycemia or hyperglycemia is essential.
-
Medication Adherence
Consistent use and timing of insulin or oral diabetic medications are critical. Missing doses or incorrect administration can significantly affect blood sugar control.
-
Psychosocial Factors
Stress, depression, and anxiety can influence blood sugar levels and management. Emotional well-being is an often overlooked but crucial component of diabetes care.
-
Dietary Management
Overall, understanding and managing blood sugar levels play a vital role in the daily lives of diabetic patients. Proper education, support, and use of monitoring technologies are invaluable in overcoming these challenges, ultimately enhancing the quality of life and reducing the risk of complications associated with diabetes.

3. The Science Behind Mindfulness and Blood Sugar Regulation
Mindfulness, a practice rooted in meditation and self-awareness, has garnered attention for its potential in managing various health conditions, including blood sugar regulation. Understanding the science behind mindfulness and its effects on blood sugar levels is crucial for those looking to harness its benefits, particularly for individuals with diabetes. This article delves into scientific studies that link mindfulness to blood sugar control, explores how mindfulness impacts stress levels and hormonal balance, and presents case studies demonstrating its benefits for diabetics.
The Science Behind Mindfulness and Blood Sugar Regulation
- Overview of Scientific Studies
- Mindfulness Impact on Stress and Hormonal Balance
- Case Studies Demonstrating Benefits
Overview of Scientific Studies Linking Mindfulness to Blood Sugar Control
Several studies have investigated the impact of mindfulness on blood sugar regulation, offering promising insights. Research suggests that mindfulness can positively influence glycemic control among individuals with diabetes. Here are some noteworthy findings:
- Mind-Body Connection: A study published in the journal Diabetes Care found that individuals who practiced mindfulness-based stress reduction (MBSR) showed improved blood sugar control compared to those who did not engage in mindfulness practices. The study concluded that the mind-body connection plays a vital role in managing diabetes.
- Reduction in A1C Levels: Another study in The Journal of Alternative and Complementary Medicine indicated that participants engaged in mindfulness practices experienced a statistically significant reduction in hemoglobin A1C levels. This metric is crucial for long-term glucose control.
- Improved Lifestyle Choices: Mindfulness has also been linked to healthier lifestyle choices. Research demonstrates that mindful individuals often adopt balanced diets and regular exercise routines, which are critical for blood sugar management.
How Mindfulness Affects Stress Levels and Hormonal Balance, Impacting Glucose Metabolism
Stress is a significant factor influencing blood glucose levels. When the body is stressed, it triggers the release of hormones like cortisol and adrenaline, which can raise blood sugar. Mindfulness practices have been shown to mitigate stress and promote hormonal balance:
- Stress Reduction: Mindfulness helps individuals cultivate a state of calm, reducing the production of stress hormones. A reduction in stress directly correlates with stabilization in glucose levels, owing to decreased cortisol secretion.
- Influence on Hormonal Balance: By promoting relaxation, mindfulness affects the hypothalamic-pituitary-adrenal (HPA) axis, responsible for regulating stress response. This leads to a more balanced hormonal system, which is beneficial for glucose metabolism.
- Autonomic Nervous System Regulation: Mindfulness enhances parasympathetic nervous system activity, commonly known as the “rest and digest” system. This supports efficient digestion and glucose processing in the body.
Example Case Studies or Findings Demonstrating Mindfulness Benefits for Diabetics
Real-world applications of mindfulness in diabetes management further underscore its potential. Let’s consider some key examples:
- Case Study: Group Mindfulness Sessions
- Finding: Long-term Benefits
A pilot program involved diabetics participating in group mindfulness sessions over eight weeks. The results showed significant improvements in participants’ fasting blood glucose levels. Participants also reported lower stress and enhanced well-being.
A longitudinal study followed individuals with type 2 diabetes who incorporated mindfulness meditation into their daily routine for over a year. The study found sustained improvements in blood glucose levels and a reduction in diabetes-related complications over time.
To conclude, mindfulness emerges as a promising adjunct therapy for regulating blood sugar. It helps in stress reduction, hormonal balance, and adopting healthier lifestyles, leading to better glucose management, especially for diabetics. Through ongoing research and practical applications, mindfulness may play a vital role in diabetes care strategies moving forward.
4. Practical Mindfulness Techniques for Diabetic Patients
Living with diabetes requires diligent management and often invokes a myriad of lifestyle changes. However, from adjusting diet and maintaining physical activity to monitoring blood sugar levels, the demands can sometimes feel overwhelming. In the realm of managing diabetes, mindfulness techniques are emerging as a compelling strategy. Practicing mindfulness not only helps with mental clarity and stress reduction but also promotes a healthier relationship with food and physical well-being. This article explores various mindfulness techniques tailored for diabetic patients, offering step-by-step guidance on incorporating them into daily routines, and tips for seamlessly merging them with diabetes management plans.
Introduction to Mindfulness Techniques
- Meditation: Meditation is a common mindfulness technique that involves focusing your mind on a particular object, thought, or activity. This practice encourages heightened awareness and mental clarity. For diabetic patients, meditation can aid in reducing stress, which is crucial as stress can directly affect blood sugar levels.
- Mindful Eating: Mindful eating involves paying full attention to the experience of eating and drinking, both in terms of physical and emotional responses. It encourages a focus on the flavors, textures, and scents of food, which can improve digestion and satisfaction and prevent overeating.
- Breathing Exercises: This technique involves performing a series of structured breathing patterns to increase mindfulness and reduce anxiety. For diabetics, controlled breathing can be a fundamental strategy to stabilize emotional responses and, by extension, blood sugar levels.
Step-by-Step Guidance on Incorporating Mindfulness
- Start with Simple Breathing Exercises:
- Find a quiet place and sit comfortably.
- Close your eyes and take deep breaths, inhaling slowly through your nose and exhaling through your mouth.
- Focus on the flow of your breath entering and leaving your body.
- Repeat this process for five minutes daily and gradually increase the duration.
- Practice Mindful Eating:
- Begin by eliminating distractions like television or mobile devices during meals.
- Before eating, take a moment to express gratitude for the food in front of you.
- Pay attention to colors, smells, and textures as you slowly chew each bite.
- Notice how the food makes you feel, both emotionally and physically. Adjust your portions and choices to reflect a balance that promotes well-being.
- Schedule Meditation Sessions:
- Set aside 10-15 minutes each day for meditation, either at the start or end of your day.
- Choose a comfortable position, either sitting or lying down, and close your eyes.
- Focus your attention on a singular thing – a word, a phrase, or your breath.
- If your thoughts wander, gently guide them back without judgment.
Tips for Integrating Mindfulness with Diabetes Management
Integrating mindfulness practices into your diabetes management plan doesn’t have to be a daunting task. Here’s how you can seamlessly bring mindfulness into your everyday life:
- Create a Routine: Consistency is essential for mindfulness practice. Choose specific times for meditation, mindful eating, and breathing exercises, ensuring they align with your meal schedules or medication regimen.
- Mindful Monitoring: Apply mindfulness when checking your blood sugar levels. Be fully present and take note of how your body feels, using this data to make informed choices about meals and activities.
- Stress Inventory: Identify potential stressors in your daily life and apply breathing techniques to address them promptly. Mindfulness helps in recognizing stress triggers and managing your responses to them effectively.
- Integrate with Physical Activity: Physical exercise is a critical component of diabetes management. Combine this with mindfulness by engaging in activities like yoga or tai chi, which naturally incorporate breathing and meditation.
- Customize Your Practice: Everyone’s diabetes journey is unique. Tailor mindfulness techniques to suit your lifestyle. Whether it’s through a walking meditation or a quiet moment before a meal, find what works best for you.
With a dedicated approach, mindfulness can become a powerful ally in managing diabetes. By integrating practices like meditation, mindful eating, and focused breathing into your routine, you can improve not just your mental well-being but also your physical health outcomes. Embrace mindfulness as a central pillar of holistic diabetes care, and notice the transformation in your daily life.