Traveling with Confidence: Tips for Managing Your Insulin While Away from Home
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to Traveling with Insulin
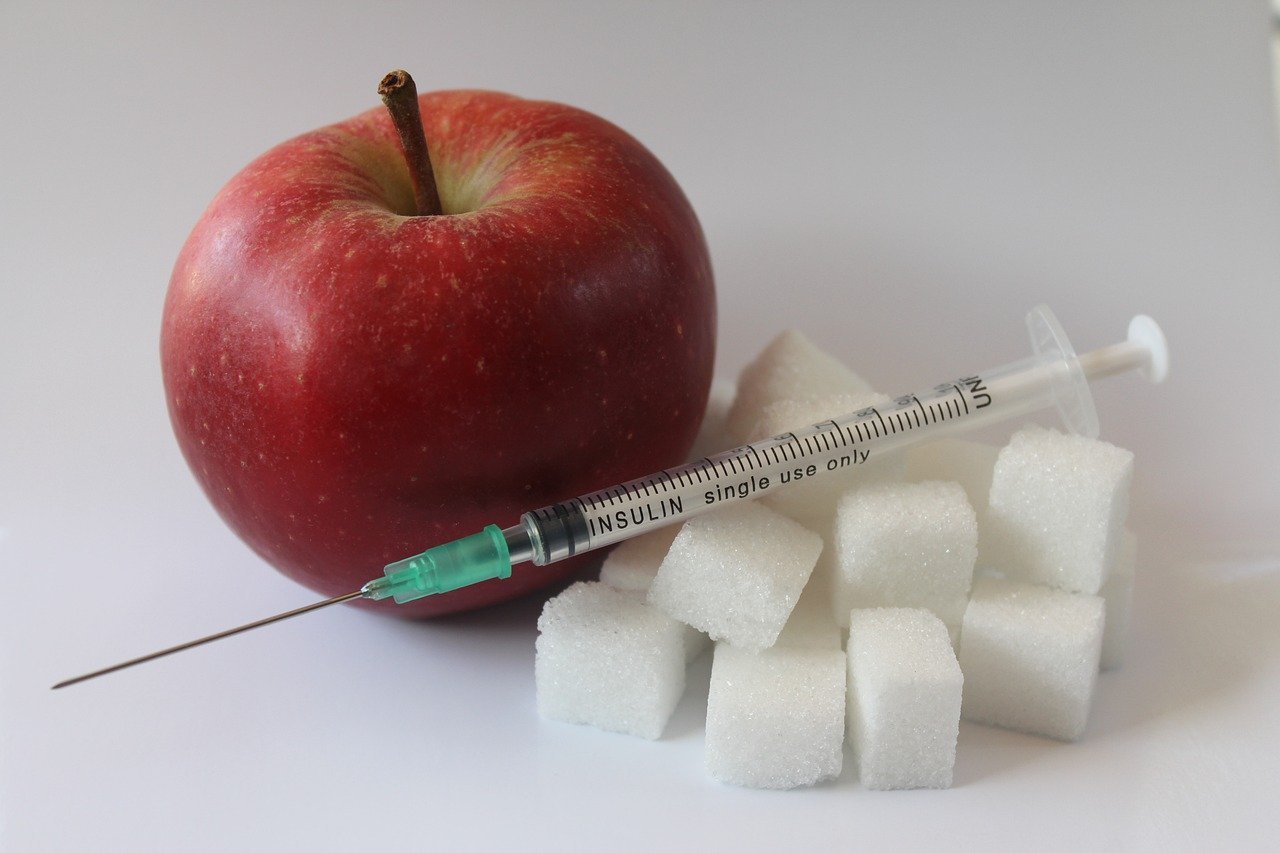
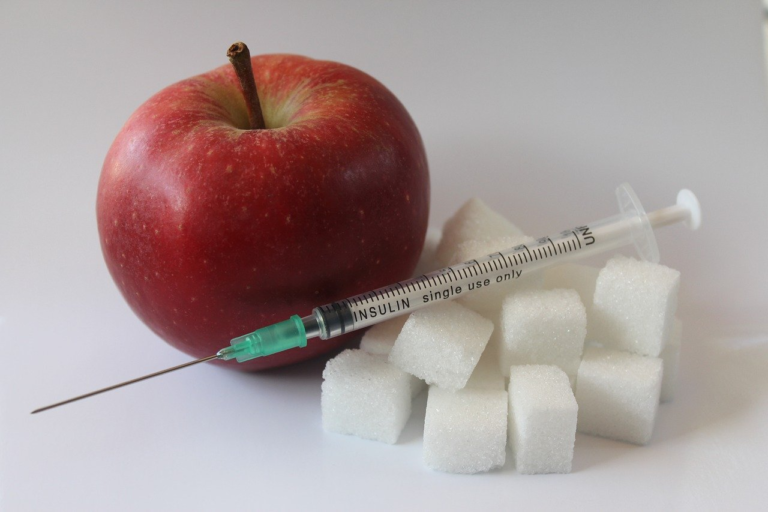
Traveling can be one of life’s most enriching experiences, offering the chance to explore new cultures, savor diverse cuisines, and create lasting memories. For individuals who are insulin-dependent, maintaining effective diabetes management while on the road is paramount. Traveling with insulin demands careful planning and consideration, yet it shouldn’t deter anyone from embarking on adventures. In this comprehensive guide, we delve into the intricacies of traveling with insulin, shedding light on the challenges and providing strategies to ensure a stress-free journey.
The Importance of Maintaining Diabetes Management While Traveling
Understanding the significance of diabetes management in daily life is fundamental, and this extends to travel situations. Managing blood sugar levels is crucial for preventing complications such as hypoglycemia or hyperglycemia. Changes in routine, diet, and activity levels during travel can considerably affect diabetes management.
- Consistent insulin administration is vital to keep glucose levels within the target range.
- Monitoring glucose levels more often helps in adapting to the travel itinerary.
- A well-structured plan contributes to peace of mind and ensures unforeseen interruptions don’t derail health.
Effective diabetes management on the move is a balancing act but one that is entirely achievable with proper preparation and knowledge. Let’s explore the potential challenges that insulin-dependent travelers often face and how to address them.
Challenges and Common Concerns Faced by Insulin-Dependent Travelers
Traveling comes with its unique set of hurdles, and managing diabetes adds an additional layer of complexity. Below are some of the common concerns:
-
Insulin Transport and Storage:
- Temperature control is critical. Insulin must be kept cool, which can be challenging without proper equipment.
- Ensure availability of refrigeration or portable coolers during your journey.
-
Time Zone Adjustments:
- Time zone changes can disrupt your insulin schedule. Adjust doses to fit the local time of your destination.
- Consult with your healthcare provider for personalized advice.
-
Security Checks and Insulin Supplies:
- Security procedures at airports may raise concerns over personal belongings, including insulin and related supplies.
- Always carry a doctor’s note and prescriptions to verify the need for medical equipment.
-
Dietary Changes:
- Exploring new cuisines can lead to unpredictable carbohydrate intake.
- Researching meal options and having carbohydrate-counting tools on hand is beneficial.
-
Language Barriers:
- Language differences may hinder communication regarding dietary needs or medical assistance.
- Learn essential phrases and carry translated medical instructions if traveling abroad.
-
Emergency Situations:
- Planning for emergencies is crucial, including knowing local medical facilities and having travel insurance.
- Traveling with a partner who understands diabetes management can be reassuring.
These challenges underscore the need for meticulous preparation, ensuring insulin-dependent travelers can navigate them smoothly, laying the groundwork for a fulfilling trip.
Traveling Confidently and Stress-Free
A primary goal for any traveler, particularly those managing a health condition such as diabetes, is to experience the journey with confidence and minimal stress. Here are several strategies to help achieve this goal:
-
Pre-Travel Planning:
- Create a comprehensive travel checklist that includes all necessary diabetes supplies.
- Inform travel companions about your condition and educate them on basic diabetes management.
-
Utilize Technology:
- Leverage apps and devices designed to help manage diabetes, such as glucose monitors or insulin pumps.
- Install travel apps that provide local healthcare information.
-
Stay Informed:
- Stay updated on travel advisories and regulations related to medical devices or medications.
- Read about recent experiences of other diabetic travelers for real-world insights.
-
Practice Self-Care:
- Ensure adequate rest and hydration to combat travel fatigue.
- Take time to unwind and enjoy the local surroundings, reducing travel stress.
Traveling with diabetes doesn’t have to be daunting. With a strategic approach, it is entirely possible to travel confidently and enjoy every moment, ensuring a trip that is both memorable and medically safe. By understanding the potential challenges and preparing adequately, insulin-dependent travelers can embark on their adventures equipped with the tools and confidence needed to keep their health in check.
Embarking on a new journey, be it for leisure or business, should be an experience filled with excitement and possibilities, without the overshadow of health concerns. Through heightened awareness and strategic planning, individuals managing diabetes can transform travel from a source of stress to a source of joy, enabling them to explore the world and its wonders with confidence.
Whether it’s a domestic weekend getaway or an international expedition, being prepared is the key to a successful and enjoyable journey. By incorporating the strategies and wisdom outlined here, travelers with diabetes can ensure that their travel stories are about the incredible destinations and experiences, not the challenges of managing their condition on the go.

2. Pre
Traveling with diabetes requires thoughtful planning and preparation, especially for those who depend on insulin. Being well-prepared can help ensure a safe and enjoyable journey without any unnecessary stress or health risks. If you’re an insulin user planning your next adventure, follow these vital steps before you hit the road. In this guide, we’ll create a comprehensive checklist for all necessary diabetes supplies, discuss the importance of consulting with healthcare providers, and explore travel-friendly medical identification options. Let’s dive into the essential pre-travel preparations for insulin users.
Checklist for Necessary Diabetes Supplies
Having a detailed checklist is crucial for ensuring that you don’t forget any essential diabetes supplies when traveling. Here’s a comprehensive list to help you prepare:
- Insulin and Delivery Devices:
- Ample supply of insulin vials/pens (consider bringing extra in case of emergencies)
- Insulin pump supplies (if you use a pump), including infusion sets, cartridges, and batteries
- Syringes or pen needles
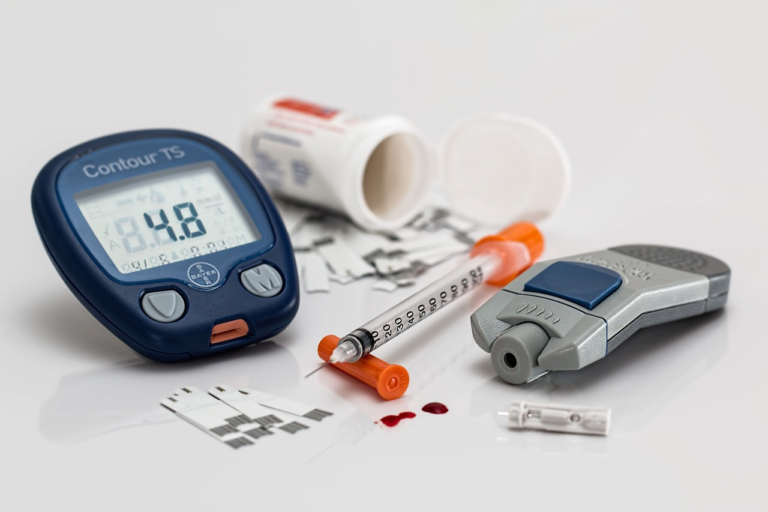
- Glucose Monitoring Supplies:
- Blood glucose meter and extra batteries
- Test strips (bring more than you think you’ll need)
- Lancets and a lancing device
- Insulin Storage Solutions:
- Insulated bag or cooler pack for keeping insulin at a safe temperature during transit
- Ice packs or gel packs to maintain temperature (consider regulations for flights)
- Emergency Items:
- Glucagon kit for severe hypoglycemia
- Fast-acting glucose (glucose tablets or gel)
- Snacks and/or glucose drinks for managing blood sugar
- Documentation and Identification:
- Doctor’s note explaining your condition and need for insulin and associated equipment
- Prescriptions for all diabetes medications
- Medical identification (bracelet or card; more on this later)
- Other Essentials:
- Backup supplies in case of loss or damage
- Contact details for healthcare providers
- Copies of any important medical records
The Significance of Consulting with Healthcare Providers
Before embarking on your journey, it’s essential to have a conversation with your healthcare provider. Here’s why consulting with them holds significant value:
- Custom Advice: Healthcare providers can offer personalized advice based on your medical history and current health status. They may recommend specific precautions or adjustments to your diabetes management plan for the duration of your travel.
- Prescription Planning: Your doctor can ensure you have enough prescription supplies and won’t run out mid-trip. They can also provide prescriptions for emergencies if you lose your supplies.
- Addressing Potential Issues: Discuss any concerns about time zone changes, dietary adjustments, or other factors that may affect your blood sugar levels while traveling. Your healthcare provider can help you create a strategy to maintain control over your diabetes.
- Vaccinations and Recommendations: Depending on your travel destination, your doctor might suggest vaccinations or other preventive measures.
- Emergency Plan: Establishing an emergency plan with your healthcare provider can give you peace of mind. Know what steps to take if you experience severe hypoglycemia or other diabetic emergencies.
Travel-Friendly Medical Identification Options
Having accessible medical identification is vital for insulin users while traveling. Medical IDs can alert others to your condition in emergencies, aiding quick and effective response. Here are some travel-friendly options:
- Medical Alert Bracelets:
- These bracelets are designed to be easily recognizable by medical personnel. They typically feature the internationally recognized medical symbol and engrave key information about your condition.
- Consider bracelets made from durable materials that can withstand different weather conditions and activities.
- Medical ID Cards:
- Carry a wallet-sized card that contains comprehensive medical information such as your diagnosis, medications, allergies, and emergency contact.
- Ensure it’s visible and accessible in your wallet or bag.
- Technology-Enabled Solutions:
- Some medical IDs now come as USBs, which may include detailed digital health information that healthcare professionals can access.
- Mobile applications that display your medical ID on your device’s lock screen are also an innovative option.
By following these pre-travel preparations, insulin users can adequately manage their condition with confidence while enjoying their travel experiences. Preparing a detailed checklist, consulting healthcare professionals, and utilizing medical identification are essential steps that together ensure a safe and successful trip. By prioritizing these preparations, you can focus more on the joy of travel and less on the challenges associated with managing diabetes on the go.

3. Navigating Transportation with Insulin
Navigating transportation with insulin can often seem daunting, whether you’re flying across the country or embarking on a long road trip. Proper planning and preparation are crucial to ensure your insulin and diabetes supplies are handled safely and efficiently during your travels. This comprehensive guide will provide valuable tips for packing and organizing insulin for air travel, explain TSA guidelines, and advise on storing insulin during extended flights or car trips.
Packing and Organizing Insulin and Supplies for Air Travel
Travelers with diabetes must carry essential insulin and supplies securely and in a manner that allows for easy access throughout their journey. Here are some strategic tips to help you pack your essentials:
- Prepare a Packing Checklist: Start by making a detailed checklist of all necessary items, including insulin, syringes, test strips, and a blood glucose meter. This ensures nothing is left behind.
- Use Insulated Bags: Insulin must be kept at a stable temperature to maintain its efficacy. Insulated bags or specific diabetes travel kits can help regulate temperatures during your flight.
- Carry Extra Supplies: Always pack more insulin and supplies than you think you will need, as unexpected delays or changes in plans can occur. A good rule of thumb is to bring double the supplies you would typically use.
- Organize with Clear Labels: Clearly label your supplies and keep them well-organized within your carry-on luggage. Transparent pouches or zip-lock bags can help segregate different items, making them more accessible when needed.
- Consider a Fridge Thermometer: If you’re carrying insulin in a thermal bag, using a small portable fridge thermometer can help ensure the temperature remains optimal throughout your journey.
TSA Guidelines for Traveling with Insulin and Other Diabetes Supplies
The Transportation Security Administration (TSA) has specific guidelines to ensure your insulin and other diabetes supplies can travel with you safely. Here’s what you need to know:
- Security Screening: Notify the TSA agent about your diabetes medical conditions and the need to carry insulin before the screening process begins. Insulin pumps and glucose monitors can remain attached to your body but should be clearly declared to the officers.
- Medical Supplies: Insulin, whether in liquid form or any other, is exempt from the 3.4-ounce liquid rule. However, it should be clearly labeled and, when possible, kept in its original packaging with a prescription label.
- Separate Inspection: Request that insulin and supplies be visually inspected, rather than x-rayed, if you are concerned about the screening equipment affecting them.
- Insulin Cooling Devices: Gel packs, freezer packs, and other liquids for regulating insulin temperature are permitted. Again, inform security personnel of these items during check-ins for easier processing.
Storing Insulin During Long Flights or Car Trips
Once you have boarded your flight or hit the road, how you store your insulin is critical to its efficacy and your peace of mind:
- Inflight Considerations: Always store your insulin with you rather than in checked baggage, where temperature fluctuations can occur. During flights, keep an eye on temperature settings, especially if flying through regions with extreme climates.
- Using Medicool Packs: When traveling by car, apply the same insulated packaging principles as air travel. Ideally, a cooler can maintain insulin at the recommended temperature of 36°F to 46°F (2°C to 8°C).
- Avoiding Extreme Temperatures: Never leave insulin in a vehicle or luggage under direct sunlight as temperatures can soar unpredictably. When you’re on a break, take your insulin with you to keep it in a more controlled environment.
- Monitor Expiration Dates: Be mindful of insulin expiration dates. The potency of insulin is compromised past its expiration or if it has been open and unrefrigerated for more than the recomended duration dictated by the manufacturer.
- Medic Alert and Documentation: Always carry your Medical Identification along with a note from your healthcare provider. It’s helpful to have this documentation on hand in case there’s a need to explain your medical situation and the need for your supplies during your travel.
Traveling with insulin does require some level of planning, but with the right strategies, it can be done smoothly and without added stress. Whether it’s packing appropriately, understanding TSA regulations, or knowing how best to store insulin during transit, a well-prepared trip can help you maintain your health regime virtually unaffected as you explore new destinations.
4. Managing Insulin and Blood Sugar While at Your Destination
Traveling with diabetes requires meticulous preparation and planning, particularly in managing insulin and blood sugar levels efficiently while you’re at your destination. Navigating through different time zones and climates can significantly affect your insulin doses and blood sugar regulation. Here’s a comprehensive guide to help you manage your diabetes effectively during your travels.
Adjusting Insulin Doses in Different Time Zones and Climates
Traveling across time zones can be challenging for individuals with diabetes due to the potential impact on insulin administration schedules. The key is to adjust your insulin doses meticulously as you transition into a new time zone. Here are some strategies you can employ:
- Consult with Your Healthcare Provider: Before you travel, discuss your travel itinerary with your healthcare provider. They can provide customized advice based on your insulin regimen and usually recommend a gradual adjustment of your insulin schedule to align with your destination’s timezone.
- Gradual Adjustment: Start adjusting your insulin schedule a few days before your trip. Gradually shift the timing of your insulin doses closer to the time you’ll need them at your destination. This slow adjustment helps your body acclimate without dramatic changes.
- Monitor and Adjust According to Climate: Warmer climates may enhance insulin absorption while colder climates may slow it down. Observe your blood sugar levels closely when you arrive and make adjustments as needed. Ensure you keep your insulin stored appropriately to maintain its efficacy.
Dining Tips to Maintain Blood Sugar Levels with New Cuisines
Exploring new cuisines is one of the joyous aspects of travel. However, it’s essential to keep your blood sugar levels stable to maintain your health. Follow these dining tips:
- Research and Plan Ahead: Research the local cuisine beforehand to identify which dishes might affect your blood sugar levels. Look for restaurants that offer online menus to choose healthier options in advance.
- Portion Control: Keep your portion sizes in check. Share meals with your travel companions or opt for starters instead of full-sized entrees to prevent overeating.
- Balance with Vegetables: Make sure to include plenty of low-carb vegetables in your meals, which can provide necessary nutrients without spiking blood sugar levels.
- Mind Your Carbohydrates: Choose complex carbohydrates like whole grains over simple carbs. Keep track of carbohydrate intake to adjust insulin doses accordingly.
- Stay Hydrated: Proper hydration is crucial, especially in hot climates, as dehydration can cause spikes in blood sugar levels.
- Pack Snacks: Carry healthy, diabetes-friendly snacks like nuts or seed bars to prevent hypoglycemic episodes while exploring.
Monitoring Blood Glucose Levels Frequently and Accurately
Monitoring your blood glucose levels is critical during travel to ensure your safety and comfort. Here’s how you can maintain accurate measurements:
- Bring Extra Supplies: Pack more than enough test strips, lancets, and batteries for your glucose meter to avoid running out.
- Invest in a Continuous Glucose Monitor (CGM): A CGM can provide real-time blood sugar readings and alerts, making it easier to monitor your levels as you travel.
- Set Timers for Testing: Use your smartphone or watch to set reminders for testing your blood sugar levels. Frequent monitoring is essential as you adjust to a new environment and schedule.
- Keep a Log: Document your blood sugar levels, noting any fluctuations, and correlate these with meal timings and types of foods consumed.
- Account for Physical Activity: Increased physical activity can lower blood sugar levels, so adjust your testing and insulin accordingly.
By implementing these strategies, you can successfully manage your insulin and blood sugar levels while enjoying your travels. Always be prepared with the necessary supplies, stay informed about your health needs, and enjoy exploring new destinations safely.