Exploring the Correlation Between Stress, Cortisol Levels, and Blood Glucose in diabetics
#ez-toc-container {
background: #f9f9f9;
border: 1px solid #aaa;
border-radius: 4px;
-webkit-box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
box-shadow: 0 1px 1px rgba(0, 0, 0, .05);
display: table;
margin-bottom: 1em;
padding: 10px 20px 10px 10px;
position: relative;
width: auto;
}
.ez-toc-container-direction {
direction: ltr;
}
.ez-toc-list-level-1 a{
font-weight:bold;
}
Table of Contents
1. Introduction to the Connection Between Stress, Cortisol, and Blood Glucose
Stress is an unavoidable aspect of modern life, affecting individuals across the globe irrespective of age or profession. It manifests as a physiological response to perceived threats, whether they’re real or imagined, triggering a cascade of reactions within the body. The relationship between stress, cortisol production, and blood glucose levels is an intricate one, with significant implications for health and wellbeing.
As we delve into understanding this connection, it is crucial to recognize the critical role that hormones, particularly cortisol, play in this dynamic. This stress hormone is fundamental to the body’s fight-or-flight response, instigating a host of physiological changes designed to enable survival in the face of adversity. However, prolonged stress and its resultant hormonal surges can have lasting impacts, especially concerning blood glucose management. Such an understanding is particularly pertinent in the context of diabetes, a chronic condition characterized by impaired glucose regulation.
-
Overview of Stress and Its Physiological Impacts
Stress is the body’s natural defense mechanism against threats, activating the Sympathetic Nervous System (SNS) and prompting a series of hormonal releases. When the brain perceives a stressor, it signals the adrenal glands to release adrenaline and cortisol, increasing heart rate, blood pressure, and energy supplies.
The physiological impacts of stress include:
- Energy mobilization: Stress leads to the release of glucose and fatty acids into the bloodstream to provide quick energy.
- Cardiovascular effects: Increased heart rate and blood pressure to supply more oxygen and glucose to muscles.
- Suppression of non-essential functions: Processes like digestion and reproductive activities are temporarily minimized to focus on immediate survival.
-
Introduce Cortisol as a Stress Hormone
Cortisol, often dubbed the primary ‘stress hormone,’ is secreted by the adrenal glands and plays a pivotal role in stress response. It helps maintain homeostasis by regulating various bodily functions including metabolism, inflammation, and immune responses, especially under stress.
Key functions of cortisol include:
- Regulating metabolism: Cortisol ensures that glucose is available for prolonged stress by breaking down proteins and fats.
- Suppressing inflammation: By managing the immune response, cortisol provides anti-inflammatory effects crucial during stress.
- Blood pressure regulation: Cortisol works to maintain cardiovascular functions during stress.
-
Brief Mention of Diabetes and the Significance of Blood Glucose Management
Diabetes, a metabolic disorder characterized by chronic high blood sugar levels, underscores the importance of proper blood glucose management. Stress, particularly chronic stress, can exacerbate this condition through its effects on hormonal balances and glucose metabolism.
For those with diabetes, managing cortisol levels becomes crucial because:
- Elevated blood sugar: Stress-induced cortisol can raise blood glucose levels, complicating diabetes management.
- Insulin resistance: Chronic stress may lead to increased insulin resistance, making blood sugar control more challenging.
- Increased health risks: Unmanaged blood glucose levels in diabetics heighten the risk of complications such as heart disease and neuropathy.
Understanding the link between stress, cortisol, and blood glucose is vital in developing strategies for effective diabetic care and overall health improvement.
In conclusion, the relationship between stress, cortisol, and blood glucose is multifaceted and significant. Cortisol plays an essential role in the body’s response to stress but also highlights the importance of managing stress to maintain healthy glucose levels, particularly for individuals with diabetes. By exploring these connections, we can better comprehend the physiological impacts of stress and the necessity of effective stress management techniques to enhance health and wellbeing.

2. Understanding Cortisol’s Role in the Body
Cortisol, often referred to as the “stress hormone,” plays a pivotal role in our body’s ability to manage stress. It is produced by the adrenal glands, which are situated on top of the kidneys. This hormone is crucial not only during periods of heightened stress but also plays vital roles in regulating various bodily functions, including metabolism, immune response, and inflammation reduction. Here we delve into the intricacies of cortisol production, its effects on bodily systems, particularly in glucose metabolism, and the significance of monitoring cortisol levels, especially for individuals with diabetes.
Understanding Cortisol Production and Regulation in Response to Stress
The production and release of cortisol follow a sophisticated process orchestrated by the hypothalamic-pituitary-adrenal (HPA) axis. Here’s how it works:
- The hypothalamus detects stress stimuli and releases corticotropin-releasing hormone (CRH).
- CRH stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH).
- ACTH travels through the bloodstream to the adrenal glands, prompting them to produce cortisol.
Once released, cortisol helps the body respond to stress by increasing glucose availability, enhancing the brain’s use of glucose, and curbing non-essential functions in the flight-or-fight response. Cortisol levels typically peak in the early morning and decline throughout the day, a pattern known as the diurnal rhythm.
Regulation Mechanism
Cortisol regulation is a dynamic feedback loop. High levels of cortisol in the bloodstream signal to the hypothalamus and pituitary to reduce CRH and ACTH production, lowering cortisol levels. Conversely, low cortisol levels prompt increased production of CRH and ACTH, boosting cortisol synthesis. This feedback system helps maintain cortisol balance and, consequently, overall homeostasis.
Effects of Cortisol on Body Systems
Impacts on Glucose Metabolism
Cortisol significantly influences how the body processes and utilizes glucose. It promotes gluconeogenesis, the synthesis of glucose from non-carbohydrate sources, in the liver, providing an energy supply during stress when glucose levels might be low.
- Blood Glucose Levels: Cortisol increases blood sugar levels by inhibiting insulin production, ensuring that enough glucose is available for muscle and brain activity during stress.
- Insulin Sensitivity: Chronic high cortisol may reduce insulin sensitivity, leading to elevated blood sugar levels and increased risk of diabetes.
Thus, while cortisol is crucial for quick energy during acute stress, prolonged elevated levels can disrupt glucose metabolism, contributing to metabolic disorders.
Other Bodily Systems Affected by Cortisol
- Immune System: Cortisol suppresses inflammation and modulates the immune response. While beneficial in short bursts, long-term elevation can weaken immune defenses.
- Cardiovascular System: Cortisol helps regulate blood pressure. However, excessive levels may contribute to hypertension and cardiovascular disorders.
- Digestive System: Stress-induced cortisol release can affect gut motility and digestion, sometimes leading to gastrointestinal issues.
Importance of Cortisol Monitoring in Individuals with Diabetes
For those with diabetes, especially type 2, monitoring cortisol levels is critical. Here’s why:
- Blood Glucose Control: High cortisol levels can complicate blood sugar management, exacerbating hyperglycemia. Understanding cortisol fluctuations helps in tailoring effective diabetes management plans.
- Insulin Resistance: Elevated cortisol can decrease insulin sensitivity, making it challenging for diabetics to maintain target blood glucose levels. Monitoring hormone levels can aid in adjusting treatments accordingly.
- Risk of Complications: Unchecked cortisol can accelerate complications associated with diabetes, such as nephropathy and neuropathy. Regular assessments can prompt proactive measures.
To effectively monitor cortisol, healthcare providers may recommend saliva, blood, or urine tests, which can then inform both stress management and diabetes treatment strategies. In particular, lifestyle modifications such as stress-reduction techniques, diet changes, and exercise can play a role in regulating cortisol production and thereby improving diabetic health outcomes.
In conclusion, understanding cortisol and its multifaceted impacts on the body, especially concerning glucose metabolism, is crucial. For individuals with diabetes, regular monitoring of cortisol levels offers a proactive measure to enhance disease management, minimize complications, and improve overall quality of life.

3. How Stress Affects Blood Glucose Levels in Diabetics
Introduction
Understanding how stress impacts blood glucose levels in diabetics requires diving into the biological mechanisms, research studies, and the real-world implications for individuals managing diabetes. In this comprehensive exploration, we will uncover the intricate relationship between stress and blood glucose, highlighted by cortisol production and its effects. For diabetics, stress management becomes a crucial aspect of maintaining healthy glucose levels.
-
Biological Mechanism Linking Stress to Elevated Blood Glucose Levels
Stress, whether physical or emotional, triggers the body’s “fight or flight” response, leading to a cascade of hormonal changes. These responses are part of an evolutionary mechanism designed to prepare the body for an emergency, triggering the release of stress hormones like cortisol and adrenaline.
When the brain perceives stress, the hypothalamus signals the adrenal glands to secrete cortisol, a hormone that plays a vital role in the body’s stress response. Cortisol’s primary function is to increase blood sugar levels to provide immediate energy for dealing with a stressor. This occurs through several mechanisms:
- Increased Gluconeogenesis: Cortisol stimulates the liver to produce more glucose, a process called gluconeogenesis. The liver converts protein and fat into glucose, raising blood sugar levels.
- Insulin Resistance: Cortisol interferes with the action of insulin, making body cells less sensitive to it. Reduced insulin sensitivity means higher levels of glucose remain in the bloodstream.
- Reduced Glucose Uptake: Cortisol can also inhibit glucose uptake in muscle and adipose tissue, ensuring that glucose is more available in the blood when needed.
For non-diabetics, this natural response may not cause significant issues. However, for individuals with diabetes, whose metabolic control is compromised, these stress-induced changes can lead to elevated blood glucose levels, complicating diabetes management.
-
Studies Demonstrating Increased Cortisol and Glucose Levels Under Stress
A wealth of studies highlights the correlation between stress and increased blood glucose levels in diabetic patients. Here are some significant findings:
- Study on Acute Stress and Blood Glucose Levels: Researchers observed that individuals with Type 2 diabetes experienced measurable spikes in blood glucose when subjected to acute stress situations, such as public speaking or mental arithmetic tasks. These spikes were coupled with elevated cortisol levels.
- Longitudinal Analysis of Chronic Stress: Chronic stress, as seen in caregiving or demanding work environments, has been associated with sustained high levels of cortisol and glucose. In a comprehensive longitudinal study, diabetics undergoing chronic stress had higher HbA1c levels, a key indicator of long-term glucose control.
- Stress Reduction Interventions: Studies exploring the impact of stress reduction techniques such as mindfulness, yoga, and cognitive-behavioral therapy demonstrate improved glucose control, suggesting that stress management can be as crucial as diet and exercise in diabetes care.
These studies underscore the importance of understanding and managing stress for maintaining optimal glucose levels in individuals with diabetes.
-
Real-Life Implications and Challenges for Diabetics in Managing Stress-Induced Glucose Spikes
Managing stress-induced glucose spikes presents real-life challenges for diabetics. Stress is an unavoidable part of life, but its impact can be mitigated through informed strategies. Here are some practical implications and challenges faced by diabetics:
- Identifying Stressors: The first step in managing stress is identifying its sources. Diabetics need to be conscious of physical, emotional, and environmental stressors.
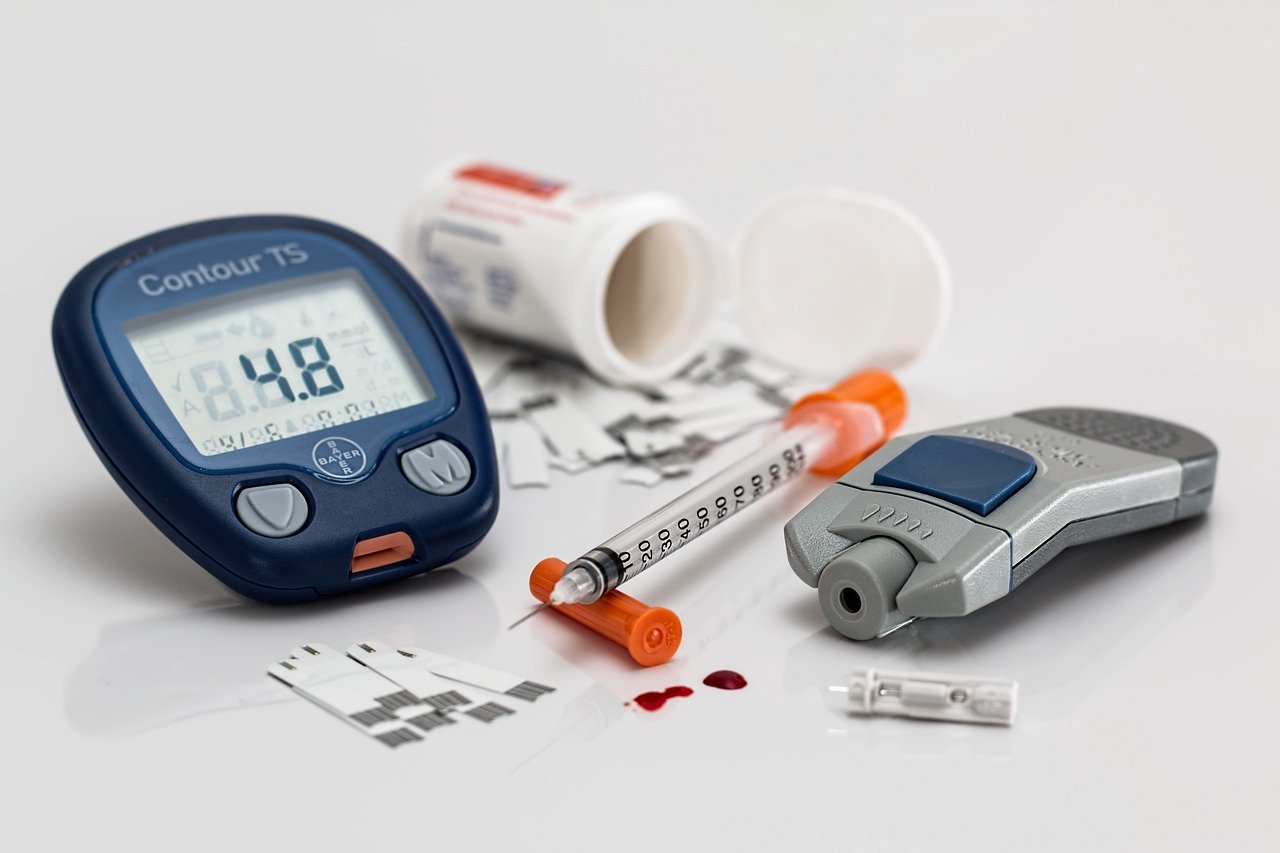
- Monitoring Glucose Levels: Frequent monitoring of blood glucose can help recognize patterns related to stress, enabling timely interventions.
- Stress Management Techniques: Techniques such as deep breathing, meditation, regular physical activity, and engaging in hobbies can help mitigate stress. Diabetics benefit from comprehensive stress management plans tailored to individual needs.
- Professional Support: Consulting healthcare professionals, counselors, and diabetes educators can provide personalized strategies to cope with stress.
- Balancing Lifestyle Factors: Achieving a balance between work, rest, and play is essential. A healthy lifestyle with adequate sleep, a balanced diet, and regular physical activity supports long-term stress management.
However, implementing these strategies can be challenging, especially in fast-paced, demanding environments. Commitment and support from family and community can play a crucial role in successful stress management for diabetics.
Conclusion
The intricate relationship between stress and blood glucose levels in diabetics is well-supported by biological insights and empirical research. Understanding the underlying mechanisms and recognizing the impact of stress on blood glucose is crucial for effective diabetes management. With carefully chosen stress management strategies, diabetics can better control stress-induced glucose spikes, contributing to improved overall health and quality of life. By prioritizing stress management along with other diabetes care strategies, individuals can navigate the challenges of diabetes with greater resilience and confidence.
4. Strategies for Managing Stress and Controlling Cortisol Levels
Stress management and maintaining optimal cortisol levels are vital for overall health and well-being. Elevated cortisol, a stress hormone, can lead to various health issues, such as weakened immune function, increased blood pressure, and disrupted sleep patterns. This segment will delve into strategies for managing stress and controlling cortisol levels, focusing on techniques such as mindfulness, exercise, dietary and lifestyle changes, and the role of medical intervention and technology.
Techniques for Stress Reduction
Incorporating effective stress reduction techniques into your daily routine can significantly impact cortisol levels and overall health. Here are some proven methods:
- Mindfulness Meditation:
Practicing mindfulness involves paying attention to the present moment without judgment. Mindfulness meditation can help decrease anxiety and stress, resulting in lower cortisol levels. Set aside as little as 10 minutes daily for mindfulness practices such as deep breathing, body scans, or guided meditation to start experiencing benefits.
- Exercise:
Regular physical activity is a powerful stress buster and a key player in balancing cortisol levels. Engaging in exercise promotes the production of endorphins, the body’s natural mood lifters. Aim for at least 150 minutes of moderate aerobic exercise, such as brisk walking or cycling, per week. Combining aerobic exercises with strength training can optimize results.
- Yoga and Tai Chi:
Both yoga and tai chi focus on breath control, gentle movements, and meditation. These practices help lower cortisol levels while enhancing flexibility, balance, and mental clarity. As little as 15-30 minutes per session, a few times a week, can contribute significantly to stress management.
Dietary and Lifestyle Changes to Support Cortisol Balance
Nutrition and lifestyle choices play a significant role in regulating cortisol levels. Implementing the following changes can help restore balance:
- Maintain a Balanced Diet:
Consume a diet rich in whole foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Nutrient-dense foods provide essential vitamins and minerals that support adrenal function, helping regulate cortisol production. Avoid excessive caffeine, sugar, and processed foods, which can spike cortisol levels.
- Stay Hydrated:
Adequate hydration is crucial for overall health and helps manage stress. Dehydration can lead to increased cortisol production, so ensure you’re drinking enough water throughout the day. Aim for at least 8-10 cups of water daily.
- Prioritize Sleep:
Quality sleep is essential for stress management and cortisol regulation. Lack of sleep can elevate cortisol levels, leading to a cycle of stress and poor rest. Aim for 7-9 hours of uninterrupted sleep per night, and establish a calming bedtime routine to improve sleep quality.
- Limit Alcohol and Nicotine:
Both alcohol and nicotine can increase cortisol levels. Reducing your intake or avoiding these substances can positively impact stress levels and overall health.
- Engage in Relaxation Activities:
Incorporate activities such as reading, listening to music, or taking warm baths into your routine. These activities can help reduce stress and promote cortisol balance.
Role of Medical Intervention and Technology in Monitoring Cortisol and Blood Glucose Levels
While lifestyle and dietary changes can significantly impact cortisol management, medical intervention and technology advances offer additional support:
- Cortisol Testing:
Regular testing can help determine cortisol levels in the body and identify any imbalances. Saliva, blood, or urine tests are commonly used to measure cortisol levels. Consulting with a healthcare provider can help interpret results and tailor a personalized stress management plan.
- Wearable Technology:
Technological advancements have made it possible to monitor cortisol levels through wearable devices. These devices can track the body’s stress response by measuring physiological markers, providing real-time feedback, and helping individuals make informed decisions about stress management.
- Continuous Glucose Monitoring (CGM):
Since cortisol also impacts blood glucose levels, monitoring blood sugar can provide additional insights into cortisol balance. Continuous glucose monitors (CGMs) offer real-time data on glucose levels, helping individuals manage stress-related glucose fluctuations.
- Medication:
In some cases, medication prescribed by a healthcare provider may be necessary to regulate cortisol levels. These treatments should be considered alongside other stress management techniques and monitored by professionals to ensure safety and effectiveness.
Managing stress and controlling cortisol levels require a comprehensive approach that integrates effective stress reduction techniques, dietary and lifestyle changes, and medical interventions when necessary. By embracing mindfulness, regular exercise, balanced nutrition, and the support of modern technology, individuals can achieve better health outcomes and enhance their quality of life.