Table of Contents
Diabetes and Varicose Veins: Recognizing the Symptoms and Seeking Treatment
Introduction
Living with diabetes and varicose veins? You’re not alone. Diabetes and varicose veins often coexist, but many are unaware of their connection. Understanding symptoms and seeking proper treatment is crucial in managing both conditions effectively. In this blog post, we will explore the relationship between diabetes and varicose veins, recognize their symptoms, discuss risk factors, delve into diagnostic procedures, cover treatment options, offer lifestyle modifications for management, and provide prevention strategies for those with diabetes – all aimed at empowering you to take control of your health! So let’s dive in and discover how to tackle this dual challenge head-on.
Understanding Diabetes and Varicose Veins
Diabetes is a chronic condition that impairs the body’s ability to regulate blood sugar levels. Consequently, it can give rise to various complications, one of which includes diabetes and varicose veins. Varicose veins are enlarged and twisted blood vessels primarily found in the legs and feet.
When diabetes is present, it can damage the blood vessels and impair circulation. This damage weakens vein walls and valves, causing restricted blood flow and increased pressure on the veins. Consequently, swelling and bulging may occur, resulting in the formation of varicose veins.
Symptoms associated with diabetes and varicose veins may manifest as pain or discomfort in the affected area, swelling, itching or tingling sensations, fatigue or heaviness in the legs. Additionally, individuals may observe visible blue or purple-colored veins beneath the skin.
Risk factors for developing diabetes and varicose veins include age, obesity, a sedentary lifestyle, pregnancy, family history of varicose veins, gender, and prolonged standing or sitting. As individuals with diabetes age, they become more susceptible to varicose veins. Excess weight places additional pressure on the legs, increasing the risk. A lack of physical activity weakens leg muscles and contributes to vein weakness. Hormonal changes during pregnancy can impact vein health as well. Additionally, having a family history of varicose veins and being female make one more prone to developing them.
Early detection and diagnosis play a vital role in effectively managing diabetes and varicose veins. If you notice any of the aforementioned symptoms or have concerns about your vein health as someone living with diabetes, it is crucial to consult your healthcare provider. They may refer you to a vascular specialist for further evaluation.
Healthcare professionals may use diagnostic procedures like ultrasound imaging to accurately assess blood flow through your limbs and identify any underlying issues contributing to your symptoms. This evaluation helps determine a customized treatment plan that suits your needs.
Treatment options for managing diabetes and varicose veins vary. Conservative measures, such as wearing compression stockings to improve circulation in the legs through external support, can be utilized. Additionally, making certain lifestyle modifications like maintaining a healthy weight and engaging in regular physical activity can also aid in management. Another recommended action is elevating the affected extremities.
Symptoms of diabetes and varicose veins
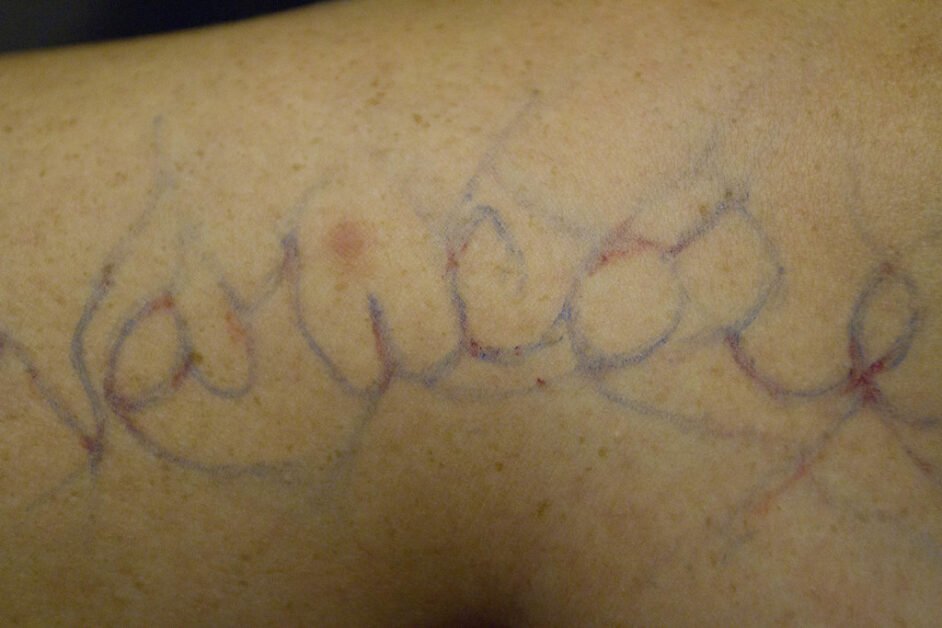
Symptoms of diabetes and varicose veins exhibit varying characteristics. However, these conditions do share common signs that individuals should be aware of. In the case of diabetes, frequent urination, excessive thirst, unexplained weight changes, fatigue, blurred vision, and slow-healing wounds may occur. On the other hand, varicose veins are characterized by bulging or twisted veins visible near the surface of the skin. These veins often appear blue or purple in color and can cause discomfort such as aching or throbbing sensations.
Individuals who have both diabetes and varicose veins must remain vigilant about any changes in their condition. Such changes may manifest as leg or ankle swelling, skin discoloration around affected veins, nocturnal leg cramps or restlessness. Moreover, prolonged standing or sitting may result in sensations of heaviness or fatigue in the legs.
It is important to recognize that these symptoms may not always indicate a significant issue. However, it is equally crucial not to overlook them. If you are experiencing any combination of these symptoms associated with diabetes and/or varicose veins, it is advisable to seek medical advice from a healthcare professional specializing in vein disorders. They will provide proper evaluation and diagnosis.
Early detection is crucial for effectively managing diabetes and varicose veins. Remember, the sooner they are detected, the better!
Risk Factors for Varicose Veins in Diabetes Patients
Diabetes and varicose veins may appear unrelated at first glance. However, individuals with diabetes must be aware of certain risk factors that can increase the likelihood of developing varicose veins. Understanding these risk factors is paramount in effectively managing one’s health.
One common risk factor for individuals is poor circulation. When someone has diabetes, it can negatively impact blood flow, causing it to slow down and resulting in a buildup of pressure within the veins. This heightened pressure places strain on the vein walls, making them more vulnerable to enlarging and twisting.
Obesity is another factor that contributes to the struggle of many diabetes patients with weight management. This struggle arises from insulin resistance or other metabolic issues. Furthermore, excessive weight adds stress to the veins, thereby increasing the likelihood of developing varicose veins.
Lack of physical activity poses a significant risk for both diabetes and varicose veins. Engaging in regular exercise not only improves blood circulation but also strengthens vein walls, ultimately lowering the probability of developing venous insufficiency.
Genetics also contribute to the likelihood of developing varicose veins. If you have a family history of this condition, particularly when coupled with diabetes, it is crucial to be extra diligent in preventing its onset.
As individuals age, their susceptibility to both diabetes and varicose veins tends to increase. This is attributed to the natural decline in elasticity of blood vessels and reduced efficiency in pumping blood back towards the heart.
Being aware of the potential risk factors linked to diabetes and varicose veins empowers individuals to proactively prevent or intervene early.
Importance of Early Detection and Diagnosis
Early detection and diagnosis are vital in managing diabetes and varicose veins. By recognizing symptoms at an early stage, individuals can promptly seek appropriate treatment, effectively preventing further complications.
The ability to detect varicose veins early on brings several key benefits. By identifying signs like swollen legs or visible vein abnormalities, individuals can take proactive measures to address the condition before it worsens. Without intervention, varicose veins can cause discomfort, pain, and even ulcers. Early detection allows for effective management and minimizes potential complications.
Early detection plays a vital role in understanding the root cause of diabetes and varicose veins. Diabetes can induce poor blood circulation and weaken blood vessels, thereby intensifying the risk of developing varicose veins. By identifying this correlation, healthcare professionals are empowered to administer targeted treatment approaches that simultaneously address both these conditions.
Early diagnosis aids individuals in comprehending their risk factors for developing severe complications related to varicose veins, including deep vein thrombosis (DVT). Armed with this knowledge, patients can make informed choices regarding alterations in lifestyle and preventive measures.
Detection and diagnosis of diabetes and varicose veins are crucial for effective management. Taking prompt action at the first signs of symptoms or risk factors helps individuals enhance their quality of life while reducing potential complications in the future.
Diagnostic Procedures for Varicose Veins
When diagnosing diabetes and varicose veins, healthcare professionals can employ various procedures to assess the severity of the condition and devise an appropriate treatment plan. One commonly utilized diagnostic method entails a physical examination, during which the doctor meticulously inspects the patient’s legs for any visible indications of varicose veins.
In addition to conducting a physical examination, doctors may utilize imaging tests like ultrasound. This non-invasive procedure employs sound waves to generate detailed images of your blood vessels and aids in identifying any irregularities or obstructions in the veins. By analyzing these images, medical professionals can assess the severity of varicose veins and determine if further intervention is necessary.
Venous duplex scanning is another diagnostic procedure that can be utilized. This technique combines traditional ultrasound with Doppler ultrasound technology, providing a comprehensive evaluation of both the structure and function of your veins. Through this test, detailed information regarding blood flow direction, velocity, and any potential valve dysfunction within the affected veins can be obtained.
In certain situations, your vein health may require the utilization of more advanced imaging techniques such as MRI (magnetic resonance imaging) or CT scans (computed tomography). These tests provide detailed cross-sectional images that enable doctors to assess deeper structures and identify any underlying issues contributing to your varicose veins.
In the diagnosis diabetes and varicose veins, it is crucial to recognize the uniqueness of each patient. Consequently, diagnostic procedures may vary based on individual circumstances. Your healthcare provider will collaborate with you to determine the most suitable tests for diagnosing and evaluating your specific case.
Treatment Options for Diabetes-Related Varicose Veins
When it comes to treating varicose veins associated with diabetes, there are multiple treatment options available. These can effectively relieve symptoms and enhance overall vein health. It is important to keep in mind that each person is unique, so the treatment approach may vary depending on factors such as the severity of the condition and other individual considerations.
Compression therapy is a commonly recommended treatment for varicose veins in individuals with diabetes. It involves wearing specialized stockings or socks that apply gentle pressure to the legs, promoting improved blood flow. By reducing swelling, discomfort, and the visibility of varicose veins, compression therapy offers potential relief for patients.
Sclerotherapy, another treatment option, involves the injection of a solution directly into the affected vein. This solution induces irritation and scarring within the vein, prompting its eventual closure. Smaller varicose veins or spider veins are often addressed using sclerotherapy.
In more severe cases, doctors may recommend minimally invasive procedures like endovenous laser ablation or radiofrequency ablation. These procedures utilize heat energy to close off problematic veins internally, thereby redirecting blood flow through healthier vessels.
Surgery may be necessary for individuals with significant venous insufficiency or complications from varicose veins. In these cases, surgical procedures such as ligation and stripping are performed to remove or tie off damaged veins. This helps alleviate symptoms and prevents further complications.
In managing diabetes and varicose veins, lifestyle modifications hold significance alongside medical treatments. By adopting healthy habits such as maintaining a suitable weight through balanced nutrition and regular exercise, individuals can alleviate pressure on their legs while enhancing blood circulation. Moreover, engaging in consistent physical activity contributes to the development of robust leg muscles that facilitate proper blood flow.
Individuals with both diabetes and varicose veins should collaborate closely with their healthcare provider to determine a suitable treatment plan tailored to their specific needs.
Lifestyle Modifications to Manage Varicose Veins in Diabetes
Living with diabetes can already pose numerous challenges. However, when combined with the presence of varicose veins, it becomes crucial to effectively manage both conditions. Taking proactive steps towards lifestyle modifications can significantly alleviate symptoms and prevent further complications.
Maintaining a healthy weight is crucial. It not only reduces the pressure on your legs but also improves vein problems. By adopting a balanced diet and incorporating regular exercise into your routine, you can shed those extra pounds and enhance blood circulation.
When it comes to circulation, it’s important to avoid long periods of sitting or standing if you want to manage varicose veins. If your job requires extended periods of sitting or standing, make sure to take short breaks throughout the day. Use these breaks to stretch your legs or enjoy a quick walk. This will help promote better blood flow and support vein health.
Wearing compression stockings offers excellent support for weakened veins. These specially designed stockings apply gentle pressure on the legs, helping to enhance blood flow and promote efficient circulation back to the heart.
Furthermore, it is beneficial to elevate your legs whenever possible as this can effectively reduce swelling and alleviate discomfort commonly associated with varicose veins. To achieve optimal results, try propping up your feet above heart level while resting or sleeping. This simple action promotes improved blood circulation throughout your body.
When considering your attire, it’s important to pay attention to clothing choices that allow for comfortable movement. Opt for loose-fitting garments that don’t restrict mobility around the waist or groin area. Additionally, steer clear of tight socks or leggings that could hinder proper blood circulation in the lower extremities.
These modifications to your lifestyle have multiple benefits. Not only can they help manage varicose veins, but they also contribute significantly to overall diabetes management. Remember, taking small steps today will make a significant difference in the future.
Prevention Strategies for Diabetes Patients
Individuals with diabetes must take proactive measures to prevent the occurrence of varicose veins. Utilizing effective strategies is crucial in this regard. Let’s explore some recommended approaches:
Controlling blood sugar levels is essential for preventing complications like diabetes and varicose veins. One should follow a healthy diet plan, engage in regular exercise, and take prescribed medications to effectively manage diabetes.
Staying active is crucial for managing diabetes and promoting healthy circulation while preventing varicose veins. Make sure to incorporate activities like walking, swimming, or cycling into your daily routine.
To maintain optimal leg health, it is important to maintain a healthy weight. Excessive weight places added strain on the legs and can increase the likelihood of developing varicose veins. Aiming for a balanced body weight through a nutritious diet and regular exercise is key.
To prevent negative effects of prolonged sitting or standing, individuals engaged in sedentary jobs or long periods of standing should prioritize regular breaks and movement to enhance proper blood circulation.
One effective way to improve circulation and reduce the likelihood of diabetes and varicose veins is by wearing compression stockings. These specialized garments apply gentle pressure on the legs, enhancing blood flow.
To effectively manage your diabetes and reduce the risk of experiencing discomfort from varicose veins, it is important to incorporate these prevention strategies into your overall diabetic care plan with guidance from your healthcare provider. By taking proactive measures today, you can minimize the unpleasant symptoms associated with both conditions.
Conclusion
As we conclude this discussion on diabetes and varicose veins, it is crucial to bear in mind their interconnectedness and the profound impact they can have on one’s overall well-being. By comprehending the symptoms, risk factors, and available treatments for varicose veins in individuals with diabetes, people can proactively manage their condition with efficacy.
Detection and diagnosis during the early stages are vital in preventing complications associated with both diabetes and varicose veins. If you notice any symptoms like leg pain, swelling, or visible bulging veins, it is important to promptly consult with your healthcare provider for further evaluation.
Diagnostic procedures, such as ultrasound imaging, play a vital role in identifying the underlying cause of varicose veins in individuals with diabetes. This information is crucial for determining the most suitable treatment approach.
Treatment options for diabetes-related varicose veins may involve making lifestyle changes, such as incorporating regular exercise and managing body weight. Additionally, medical interventions including compression therapy, sclerotherapy, or endovenous ablation procedures can be considered.
Incorporating healthy habits into a daily routine is crucial for managing varicose veins in individuals with diabetes. The key factors include regular exercise, maintaining a healthy weight, wearing compression stockings when necessary, and elevating the legs while resting. These practices collectively contribute to relieving symptoms and enhancing blood circulation.
Individuals with diabetes, being at a higher risk of developing varicose veins, should prioritize preventive strategies. These measures encompass maintaining blood sugar levels through dietary control and medication adherence, while also avoiding prolonged periods of immobility when sitting or standing.
Proactively recognizing the symptoms of both diabetes and varicose veins can greatly contribute to early detection and effective management without explicitly stating it. If you suspect you may have either condition, seeking professional advice promptly is essential for appropriate diagnostic tests. By taking a holistic approach, incorporating lifestyle modifications alongside medical treatments when necessary, you will be better equipped to manage this dual challenge effectively.
FAQ’s
Q: Can diabetes cause varicose veins?
A.Common symptoms of this condition include the presence of swollen and twisted veins, discomfort or pain in the legs, itching or burning sensations around the affected area, muscle cramps or aching, and skin discoloration.
Q: How are varicose veins diagnosed in individuals with diabetes?
To diagnose varicose veins, healthcare providers usually start with a physical examination and gathering your medical history. They might also suggest imaging tests like an ultrasound to assess the condition of your blood vessels.
Q: What treatment options are available for diabetes-related varicose veins?
A: Treatment options for diabetes-related varicose veins may include lifestyle modifications such as exercise and weight management, compression stockings to improve circulation, minimally invasive procedures like sclerotherapy or endovenous laser therapy (EVLT), or surgical interventions if necessary.
Q. Are there any preventive measures that individuals with diabetes can take to lower their risk of developing varicose veins?
Yes! Preventive strategies for diabetic patients include maintaining a healthy weight through tailored diet and exercise routines. It is also crucial to manage blood sugar levels by following prescribed medication regimens and regularly monitoring glucose levels.
The information presented within this article serves the sole purpose of providing informational content. It should be noted that it is not intended to substitute medical advice. In case you have concerns regarding your health or suspect a potential connection between varicose veins and diabetes, we strongly advise consulting with a qualified healthcare professional. They possess the expertise necessary to offer personalized guidance based on your specific situation.
Recognizing the symptoms early on and promptly seeking appropriate treatment options can greatly improve one’s prognosis.
Individuals with diabetes have the ability to effectively manage varicose veins, which can greatly enhance their overall quality of life.